Trigger points in the rhomboids
This is an excerpt from Soft Tissue and Trigger Point Release-2nd Edition by Jane Johnson.
Trigger points in the rhomboid muscles (figure 6.1) cause pain in the rhomboid area but can also cause symptoms in the region of the supraspinatus. The best way to palpate rhomboid muscles to locate trigger points is with the shoulder flexed and the scapula protracted. The application of STR to the rhomboid muscles lends itself well to the identification of trigger points as, whether STR is performed with the client prone (passive STR), seated (active-assisted STR), or standing (active STR), the scapula can be protracted. You can find trigger points throughout the rhomboid muscles between the medial border of the scapula and the spine. In many people, the rhomboids are lengthened and weak, so whilst STR can be applied to them, it is important to ask yourself whether it should be applied to them. Before you begin, note whether your client has a kyphotic posture, the posture associated with protraction of the scapulae with stretched and weak rhomboids. If you are not sure how assess the client's posture, refer to a text such as Postural Assessment (Johnson, 2012).
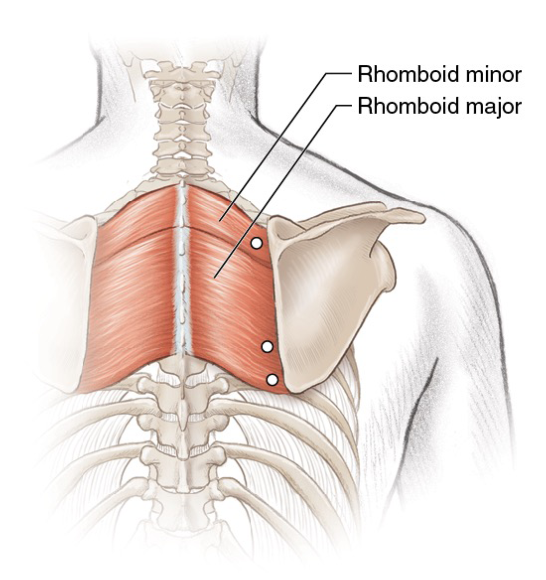
Figure 6.1 Trigger points in the rhomboid muscles.
When treating a client with a typical thoracic curve, you may apply STR to trigger points by following any of the methods (passive, active-assisted or active). Locate the trigger points and, whilst maintaining your lock, stretch the tissues. Clients with active trigger points in the rhomboid muscles often also have active points in the upper fibres of trapezius too, so to be fully effective it is important to deactivate those trigger points. If your client has a kyphotic posture, then trigger points can be deactivated through gentle pressure, but avoid overstretching the muscles afterwards. Instead, encourage your client to engage in a programme for strengthening the rhomboids and the lower fibres of trapezius.
Tewari et al. (2017) report how they deactivated two trigger points in the left rhomboids and left erector spinae of a person with Ehlers-Danlos syndrome (a form of hypermobility) who had chronic upper-back pain. They injected the triggers with lignocaine, and they prescribed the application of heat and 10 minutes of deep massage twice a day. Seven days later, the subject reported a 60 to 80 percent relief from pain, which had been measured using a visual analogue scale (VAS).
Botha (2017) compared ischaemic compression with the use of a foam roller for the deactivation of trigger points in the rhomboid muscle; 30 participants were randomly split into either the compression or foam roller group. Six treatments were delivered over a period of 6 weeks, and both subjective (questionnaire and VAS) and objective (pressure algometer) measurements were taken. Botha concluded that both treatments were equally effective at reducing trigger points with neither being superior.
SHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- Using double inclinometers to assess cervical flexion
- Trunk flexion manual muscle testing
- Using a goniometer to assess shoulder horizontal adduction
- Assessing shoulder flexion with manual muscle testing
- Sample mental health lesson plan of a skills-based approach
- Sample assessment worksheet for the skill of accessing valid and reliable resources


