Esports Players and Headaches
This is an excerpt from Conditioning for Esports by Taylor Johnson,Joanne DiFrancisco-Donoghue,Jerry Balentine.
By Mark Gugliotti, Pamela Karp, and Caitlin McGee
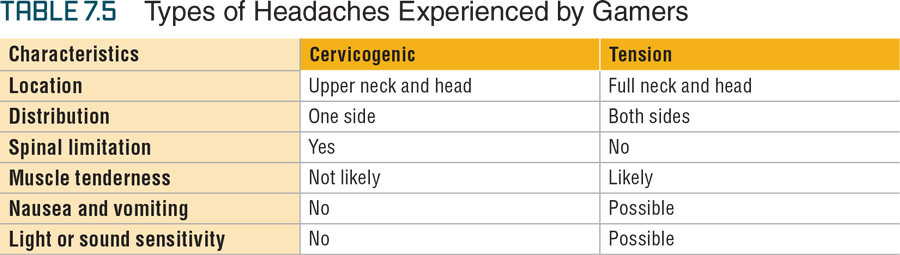
Although there are several different types of headaches, cervicogenic and tension-type headaches are the two affecting most esport athletes. Cervicogenic headaches are headaches whose problem source stem from the upper cervical spine. It is related to neck movement, compression, and motion limitation (11, 37, 40). The main contributors to cervicogenic headaches are the top three cervical segments (occiput, C1, and C2 that are directly under the skull) and their associated joints, which are the atlanto-occipital (occiput/C1) and atlantoaxial (C1/C2) joints. These joints or the spinal nerves related to these vertebral segments can cause a referral of pain to the craniofacial regions (i.e., the parts of the head enveloping the brain and the face) often along the fifth cranial nerve distribution. The pain associated with cervicogenic headaches is unilateral and varied in intensity and duration. The clinical tests used for diagnosis are beyond the scope of this chapter but include upper cervical mobility testing and the cervical flexion rotation test (70). This test is applied to the patient in a supine position. Full passive cervical flexion is followed by full rotation to both sides. Confirmation of the cervicogenic headache would require less passive rotation to the side of the headache by at least 17 degrees.
The second type of headache to consider when working with the gaming population is tension headaches. The source of these headaches is unknown, but consideration is often given to increased tension of the local muscle tissue (6, 54). These headaches are thought to be either episodic or chronic in nature. The common attributes experienced by both groups is mild or moderate pain with a bilateral pressure or tightness of the associated muscles. The episodic group experiences one episode per month lasting from 30 minutes to 7 days with possible sensitivity to light and sound but no nausea or vomiting. The chronic group experiences 3 to 15 episodes per month lasting hours or continuously with possible sensitivity to light and sound accompanied by nausea or vomiting. Manual pressure to the surrounding muscle tissue provokes their clinical symptoms (table 7.5). Interventions for both headaches include the use of medication and education to help self-manage and therapeutic modalities (e.g., electric stimulation) to dampen the pain response. Massage and manual stretching can be incorporated to elevate muscle spasms or tightness of the surrounding musculature. Gentle range of motion (ROM) exercises can be coupled with graded joint mobilization (grades 1-4) to minimize the pain response and improve mobility. Therapeutic exercise should include cervical or scapular stabilization, endurance or postural training, and progressive strengthening (10, 38).
SHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- How do I integrate nutrition education into PE?
- How does the support of friends and family influence physical activity?
- What makes the Physical Best approach unique?
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?


