Using Ultrasound as a Therapeutic Modality
This is an excerpt from Therapeutic Modalities for Musculoskeletal Injuries 4th Edition With Online Video by Craig R Denegar,Ethan Saliba,Susan Saliba.
Ultrasound
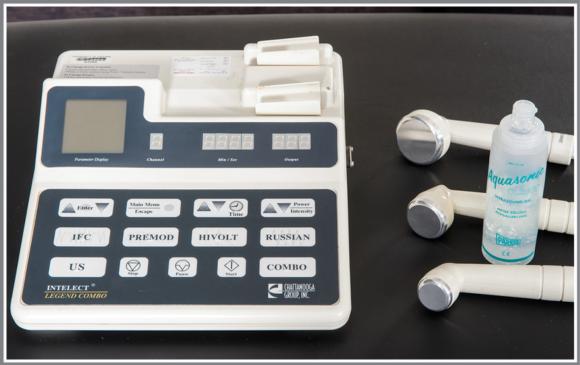
Ultrasound differs from the modalities discussed in the previous three chapters in that it transmits energy that falls within the acoustic, rather than electromagnetic, spectrum. Ultrasound is used in medicine for imaging as well as in the treatment of musculoskeletal conditions. Different frequencies of ultrasound are used for each application. The ultrasound units used in the practice of athletic training and physical therapy emit sound energy at frequencies between 800 kHz (800,000 Hz) and 3 MHz (3,000,000 Hz). Modern high-quality ultrasound units allow the clinician to select the treatment frequency. Typically a clinician can choose frequencies near 1 MHz and 3.3 MHz. Some units are also adjustable to 2 MHz (figure 12.1). The importance of frequency and the applications of ultrasound at various frequencies will be discussed in detail. Initially, it is important to understand that therapeutic ultrasound uses acoustic energy, delivered at very specific high frequencies.

Modern combination ultrasound, laser, and electrotherapy device.
Ultrasound machines use electrical current to create a mechanical vibration in a crystalline material housed in the "head" of the unit. Vibration of the crystalline material produces a wave of acoustic energy (ultrasound) (figure 12.2). The crystalline material in modern ultrasound devices is synthetic, although natural crystals were once used. The sound energy emitted from the ultrasound head travels through tissues and is absorbed.
Components of an ultrasound unit.
Ultrasound technology is now used extensively for diagnostic imaging. Ultrasound in the range of 3.5 MHz to 15 MHz is used to image organs of the abdomen and thorax as well as musculoskeletal tissues (Whittaker et al. 2007). Ultrasound is also routinely used for prenatal examination. Through ultrasound, some correctable birth defects can be identified, and the sex of the fetus can also be determined.
In musculoskeletal care, ultrasound can be used to detect muscle strains, ligament sprains, and degenerative changes in tendon. The sound energy used for imaging differs in frequency and pulse characteristics from that used for therapeutic purposes.
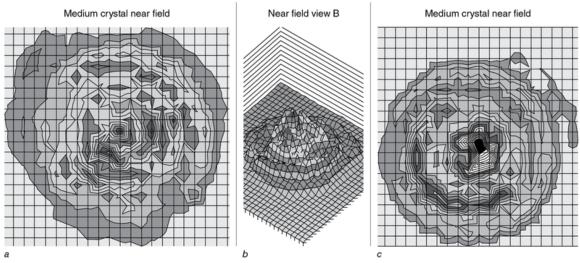
Beam Nonuniformity Ratio and Effective Radiating
Two terms describe the size and quality of an ultrasound crystal found in therapeutic ultrasound devices. Effective radiating area (ERA) is the area that receives at least 5% of the peak sound energy. This is essentially the size of the area to which sound energy is conducted when the head of the ultrasound unit contacts the skin. The ERA is somewhat smaller than the surface area of the sound head.
The beam of sound energy emitted from a crystal is not uniform but rather is characterized by areas of high intensity and lower intensity (figure 12.3). Beam nonuniformity ratio (BNR)is the ratio of the average intensity of the ultrasound beam across the ERA divided by the peak intensity of the ultrasound beam; the lower the BNR, the more uniform the intensity of the sound wave.
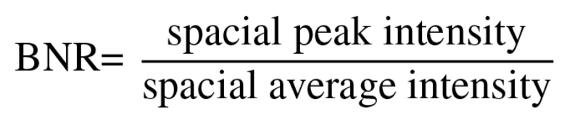
Beam scan of a crystal with a beam nonuniformity ratio (BNR) of 2.32, (a) top view and (b) side view. When tested on 40 subjects, the ultrasound transducer housing this crystal produced a very comfortable treatment at 1.5 to 2.0 watts per cm2 (W/cm2). Beam scan of a crystal with a BNR of 7.75, (c) top view. When this was tested on 40 subjects, the ultrasound transducer housing the crystal produced an uncomfortable treatment at 1.5 W/cm2 and was not tolerated at 2.0 W/cm2.
Courtesy of Brigham Young University Sports Injury Research Center.
A low BNR minimizes the risk of developing "hot spots" and allows the clinician to deliver higher doses of ultrasound without causing pain and discomfort. The BNR must be listed by the manufacturer on all units. Ideally, the BNR would be 1; however, this is impossible, and the acceptable range is between 2 and 6.
Unfortunately, BNR and ERA may not adequately define how an ultrasound unit will function. Holcomb and Joyce (2003) reported significant differences in the change in tissue temperature between two ultrasound units with a BNR of 3.7 and 2.3 and an ERA of 4.9 and 4.6 cm, respectively. These authors speculated that the area of peak intensity or peak area of the maximum beam nonuniformity ratio (PAMBNR) as described by Draper (1999) might explain why two ultrasound units differ in performance. Certainly a small spike of peak amplitude as illustrated in figure 12.4 will deliver less energy and therefore have less thermal effect than that provided by a larger area of peak amplitude. Johns, Straub, and Howard (2007) and Straub, Johns, and Howard (2008) reported considerable variability in ERA and special average intensity in 3 and 1 MHz ultrasound units, respectively, from different manufacturers. Differences between reported and actual ERA values were identified for all but one manufacturer when 3 MHz sound heads were evaluated (Johns, Straub, and Howard 2007). Demchak, Straub, and Johns (2007) noted differences in the rate but not peak heating of the calf muscles using three different 1 MHz ultrasound transducers. Johns et al. (2007), however, have reported greater heating with 1 MHz sound heads with more concentrated energy fields. The issue of equipment performance across parameters requires further study. Variability in the characteristics of the acoustic energy field may yield differing treatment effects and perhaps pose a risk of adverse events. Frye et al. (2007) reported blistering of the anterior shin after ultrasound to the calf muscles in laboratory experiments employing common clinical treatment parameters.

The area of peak intensity, (a) small and (b) larger, may affect the performance of ultrasound devices.
Conducting Media
Air is a poor conductor of ultrasound energy. To maximize delivery of sound energy to the tissues, a conducting medium must be used. Several substances have been used to conduct ultrasound, including ultrasound gel, gel pads, mineral oil, lotions, and water. The amount of sound energy conducted varies substantially between conducting media. Commercial ultrasound gel (Draper 1996; Draper et al. 1993; Klucinec et al. 2000) and gel pads (Klucinec et al. 2000; Klucinec 1996) (figure 12.5) are superior conducting media. Water is not as good a conducting medium (Draper 1996; Draper et al. 1993; Klucinec et al. 2000; Klucinec 1996; Forrest and Rosen 1989, 1992), attenuating as much as 65% of the sound energy (Klucinec et al. 2000).

Ultrasound gel and gel pads.
Rubley et al. (2008) reported smaller differences (approximately 15%) in Achilles tendon tissue heating when comparing gel and degassed water as conducting media. Differences in research methods and ultrasound equipment may explain the estimated magnitude of differences between conducting media. Collectively, however, the research suggests that ultrasound gel is the conducting medium of choice for clinical administration of therapeutic ultrasound. The conducting capacities of most gels and creams have not been established. However, some have been shown to be very poor conductors of sound energy (Cameron and Monroe 1992; Draper 1996; Draper et al. 1993; Forrest and Rosen 1989, 1992; Klucinec 1996; Klucinec et al. 2000). When applying ultrasound, use gels and gel pads known to be effective conductors.
Parameters of Treatment with Ultrasound
As with electrotherapy, you can alter the treatment parameters of ultrasound depending on the desired effect. Fortunately, the number of adjustable parameters is smaller. You can control the amplitude of the sound waves and therefore the amount of sound energy being emitted from the sound head. The sound energy emitted by the crystal is measured in watts (W). The dose of sound energy delivered is based on the amount of energy being emitted divided by the radiating area of the crystal measured in square centimeters (cm2). Thus, ultrasound dose is measured in W/cm2. You can also adjust the duty cycle, duration of treatment, and frequency.
Duty cycle refers to the process of interrupting delivery of the sound wave so that periods of sound wave emission are interspersed with periods of interruption. Figure 12.6 depicts pulsed and continuous ultrasound.

(a) In pulsed ultrasound, energy is generated only during the "on" time. Duty cycle is determined by the ratio of "on" time to pulse, in this case 50%. (b) Continuous ultrasound is shown.
Often you can select between several duty cycles. Duty cycle is calculated by dividing the time during which sound is delivered by the total time the sound head is applied. For example, if ultrasound is transmitted for 150 ms out of every second of treatment, then the duty cycle is 150/1,000, or 15%. When the emission of sound energy is not interrupted, the duty cycle equals 100%, and the ultrasound is referred to as continuous ultrasound.
Much has been learned about the treatment duration needed to elevate tissue temperatures. An interaction among the frequency, dose, and treatment duration has also been found. Some recipes for duration and intensities of ultrasound treatments used in the past do not increase tissue temperature sufficiently.
The frequency of the sound waves affects the depth at which the greatest amount of ultrasound energy is absorbed, as well as the time required to increase tissue temperature. Ultrasound units typically allow for treatment with more than one frequency, but older units had a single fixed frequency of 1 MHz. Treatments with higher frequencies are usually more appropriate for musculoskeletal injuries.
Sound Energy Absorption in Tissues
The amount of acoustic energy absorbed by tissues is influenced by many factors. The tissue characteristics, as well as the frequency, dose (W/cm2), duty cycle, and duration of treatment with ultrasound affect the amount of acoustic energy absorbed. When continuous ultrasound is delivered, the greater the energy absorption, the greater the tissue heating. Tissues with greater protein density have a higher rate of absorption, whereas tissues with a higher water content have lower absorption rates. Thus, tendon, ligament, and muscle tissue absorb more sound energy than skin and adipose tissue. Superficial bones and nerves absorb the most energy.
Ultrasound at a higher frequency (3 MHz) is absorbed more rapidly than that at a lower frequency (1 MHz) (figure 12.7). Therefore, ultrasound at higher frequencies affects tissues that are more superficial, whereas at a lower frequency less energy is absorbed superficially and more is available to penetrate into tissues. Thus, if the goal of treatment is to heat the capsular tissue at a joint such as the elbow with ultrasound, a 3 MHz frequency is appropriate. Temperature increases of up to 8°C have been reported with 3 MHz ultrasound at 1 W/cm2 in 4 min in superficial tissues such as the patellar tendon (Chan et al. 1998). If the target tissue is deep tissue, a lower frequency (1 MHz) is necessary; 10 min of continuous 1 MHz ultrasound at 2.0 W/cm2 will elevate temperature about 4°C at a depth of 2.5 cm (Draper, Castel, and Castel 1995). There is likely considerable overlap in tissue heating between 1 and 3 MHz ultrasound, as heating of tissues at 2.5 cm depths with 3 MHz ultrasound has been reported (Hayes et al. 2004). The interactions between ultrasound parameters and thermal response are discussed further shortly.
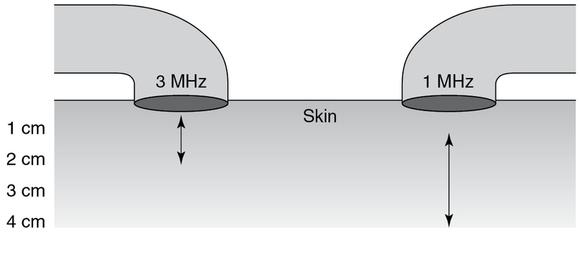
A great depth of heating is achieved with 1 MHz. The specific depth of heating is device dependent, and the values provided represent a range rather than specific limits of thermal responses.
Learn more about Therapeutic Modalities for Musculoskeletal Injuries, Fourth Edition With Online Video.
More Excerpts From Therapeutic Modalities for Musculoskeletal Injuries 4th Edition With Online VideoSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- How do I integrate nutrition education into PE?
- How does the support of friends and family influence physical activity?
- What makes the Physical Best approach unique?
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?


