Understanding and recommending exercise for clients with joint replacements
This is an excerpt from NSCA's Essentials of Training Special Populations by NSCA -National Strength & Conditioning Association,Patrick Jacobs.
Joint replacement surgery (also known as arthroplasty) involves replacement of part (e.g., articular cartilage) or all of a damaged or arthritic joint with a metal, plastic, or ceramic prosthesis in order to return the joint to normal pain-free movement (figure 3.7). While total hip and knee replacements are the most common, other joints are also replaced, including, but not limited to, shoulder, elbow, and ankle. In 2011 approximately 1.4 million joint replacement surgeries were performed in the United States, including over 640,000 knee and 300,000 hip total joint replacements. The cumulative number of individuals living in the United States with knee replacements is estimated at over 4 million, with a higher prevalence in females than males and overall prevalence increasing with age. The financial cost of joint replacements was estimated at approximately $16 billion in the United States in 2006 and was projected to rise with the increasing aging population and prevalence of obesity.
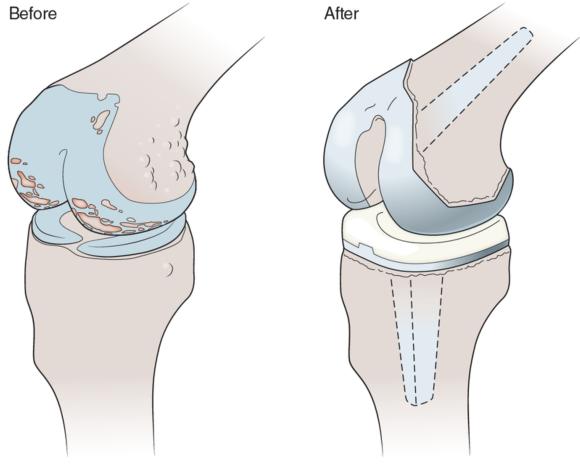
Joint replacement surgery (arthroplasty) involves replacement of part or all of a damaged joint with a metal, plastic, or ceramic prosthesis in order to return the joint to normal pain-free movement.
Pathophysiology of Joint Replacements
Several risk factors leading to joint replacement have been identified; these include age, sex, body mass index, developmental disorders, fractures, injury, and diseases leading to degeneration of one or more aspects of the joint. However, both primary and secondary OA was the principal diagnosis for 85.3% and 97.3% of hip and knee total replacement surgeries, respectively, in the United States in 2011.
Common Medications Given to Individuals With Joint Replacements
Arthroplasty is an invasive procedure, and the medications commonly associated with the surgery include anesthesia, sedatives, intravenous prescription opioid pain relievers (e.g., morphine, fentanyl, oxycodone), and antibiotics. Once the individual is released from the hospital following surgery and acute recovery, various OTC and prescription medications are prescribed (see medications table 3.4 near the end of the chapter). Over-the-counter medication for mild to moderate pain relief (e.g., acetaminophen [Tylenol]) and reducing inflammation (e.g., ibuprofen [Advil]) may be taken for up to several weeks postsurgery; however, as noted earlier, caution is advised as NSAIDs increase the risk of heart attack and stroke with higher doses and longer use. Prescription oral opioid pain relievers may be prescribed for those with more severe pain; however, extended use of these drugs is not recommended because they are highly addictive. Oral antibiotics are also typically prescribed to prophylactically prevent infections, and while side effects are not common, they may include nausea, vomiting, GI distress, or allergic reaction. Oral anticoagulants such as warfarin (Coumadin) are also commonly prescribed because surgery increases the risk of blood clots.
Effects of Exercise in Individuals With Joint Replacements
Postoperative physical activity and exercise to stimulate leg blood flow are encouraged to reduce the risk of blood clots such as deep vein thrombosis and pulmonary embolism, which are strikingly common; 40% to 60% of total hip and total knee arthroplasty patients who did not receive antithrombosis treatment had a confirmed postoperative diagnosis.
Key Point
Postoperative physical activity is encouraged in individuals with joint replacements to stimulate leg blood flow and reduce the risk of blood clots. Clearance to exercise from a physician or other health care professional should be obtained prior to initiating exercise.
Exercise Recommendations for Clients With Joint Replacements
Recovery and rehabilitation following joint replacement are highly individualized, as the healing and pain associated with the surgery can last weeks to months, as can the adjustment to the new joint and its movement. During this period of reduced activity, loss of muscle strength will accrue and should be considered and addressed. Initially the client's physician and physical therapist direct the exercise prescription to restore normal and healthy movement patterns and strengthen the joint and associated structures and musculature.
Due to the invasive nature of the surgery, the various types of joint replacement (i.e., partial or total), individualized responses to recovery and rehabilitation, and inconsistencies in the literature, specific exercise prescription is highly individualized. Following the initial recovery and rehabilitation phase, evidence of functionally stable and painless movement patterns of the affected joint is necessary before the client begins a strength and conditioning program. General guidelines for such a program include the following:
- A period of six months is recommended before engaging in vigorous exercise.
- An initial period of low-impact aerobic exercises (i.e., those that combine cyclic low limb movement patterns with low rotational and minimal impact forces) is highly recommended. This includes cycling, swimming, walking, low-impact aerobics, weight training, and cross-country skiing.
- High-impact activities and contact sports should be avoided.
- Exercise and physical activity that include frequent jumping or plyometrics are contraindicated in most cases but should be evaluated individually.
- The client's prior exercise and sporting experience should be considered in these recommendations, as this may indicate an increased tolerance for those activities.
In conjunction it is recommended that exercise professionals refer to the generally accepted guidelines adopted by the U.S. DHHS for developing exercise sessions and programs for adults with joint arthroplasty, while ensuring that the exercise prescription is individualized in its implementation and progression to reflect the limitations, strengths, weaknesses, and goals of the client. The recommendations for a resistance training program are to improve overall muscular strength and endurance; however, a loss of muscle mass may also have occurred, and if so should be addressed. Initial recommendations are two to four sets (one set if the client is sedentary or low in conditioning) of 8 to 12 repetitions per exercise at an initial light to moderate intensity, one or two times per week. To increase flexibility and range of motion it is recommended that clients initially complete static stretches three to seven times per week of all major muscle groups and hold each stretch for 15 to 30 seconds. Recommendations for aerobic exercise are to engage large muscle groups (e.g., brisk walking) at an initial light to moderate intensity for at least 10 minutes three or more times per day, three or more days per week, progressing to at least 300 minutes of moderate or 150 minutes of vigorous (or an equivalent combination of both intensities) per week. Exercise should cease immediately if there is any pain, with referral to a physician or other health care professional. Program design guidelines for clients with joint replacements are summarized in table 3.6.

Learn more about NSCA's Essentials of Training Special Populations.
More Excerpts From NSCA's Essentials of Training Special PopulationsSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- Using double inclinometers to assess cervical flexion
- Trunk flexion manual muscle testing
- Using a goniometer to assess shoulder horizontal adduction
- Assessing shoulder flexion with manual muscle testing
- Sample mental health lesson plan of a skills-based approach
- Sample assessment worksheet for the skill of accessing valid and reliable resources


