Thermoregulation Concerns
This is an excerpt from Medical Conditions in the Physically Active 4th Edition With HKPropel Access by Katie Walsh Flanagan,Micki Cuppett.
Evaporative cooling is the most effective heat loss mechanism for the body, providing more than 80% of heat loss in the able-bodied athlete. Individuals with SCI cannot depend on the autonomic nervous system to lower their core temperature by regulating blood flow. In addition, sweating is often impaired below the level of spinal cord lesion, requiring the body to rely on less surface area for evaporative cooling. Therefore, individuals with SCI are at increased risk of heat illness, and the athletic trainer must keep careful watch over athletes during high-energy sports that raise their core temperature. Individuals with tetraplegia and those with lesions above T6 are especially vulnerable to heat illness because they cannot increase the heart rate to sustain cardiac output when blood must flow to both the muscle and the skin.
Likewise, individuals with SCI may lack normal warming mechanisms, such as piloerection, shivering, and circulatory shunting, in cold conditions. A lack of working muscle mass below the level of lesion contributes to temperature regulation problems. Even temperatures around 10 °C (50 °F) may pose problems for an individual with a cervical or high thoracic lesion. Impaired or absent sensation intensifies the risk of hypothermia because these individuals may be unaware of the loss of body heat. Individuals with SCI are particularly susceptible to cold. The athlete, athletic trainer, coaches, and other team members need to be sensitive to not only the environmental conditions but also inadequate clothing, prolonged levels of inactivity during competition, improper warm-up, and dehydration.
Signs and Symptoms
Recognizing the early warning signs and symptoms of dehydration in the athlete with SCI is crucial in preventing severe complications from heat stress. Signs and symptoms include thirst, irritability, fatigue, headache, weakness, dizziness, decreased performance, erratic wheelchair propulsion, flushed skin, head or neck heat sensations, vomiting or nausea, and general discomfort. Although chills and muscle cramps are common in athletes, such signs may not be present in athletes with SCI if piloerection is impaired. Cramping of the gastrocnemius and abdominal muscles is common, but these muscles are often nonworking in athletes with SCI.
Dehydration can also occur in hyperthermal situations during cold weather or when hypothermia also exists. Dehydration causes reduced blood volume, resulting in less fluid available to cool or warm tissues. Low temperatures accentuated by wind and dampness can pose a major threat to any individual but especially to the athlete with SCI, who may lack the normative mechanisms for warming.
Referral and Diagnostic Tests
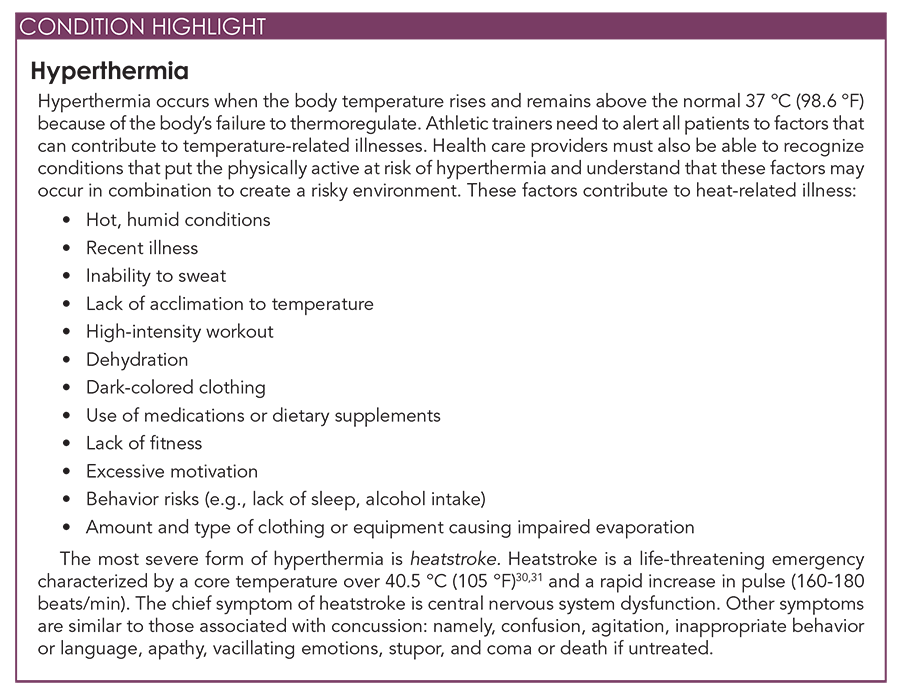
Thermoregulatory problems are often incorrectly attributed to fatigue, illness, hypoglycemic reactions, concussion, or head injury. To determine hyperthermia, the clinician checks a distressed athlete for hot skin. Because the person with SCI has a diminished ability to regulate blood flow beneath the lesion, rectal temperatures may not provide accurate readings of core temperature; studies have been successfully completed using esophageal temperatures to better determine core temperature. In addition, when the thermoregulatory system is impaired, typical signs such as shivering might not be observable. It is critical that the health care provider be able to review a thorough patient medication and nutritional supplement history that includes prescriptions and over-the-counter products. Sympathomimetics and anticholinergics affect thermoregulation, as do diuretics and excessive caffeine intake. Emergency referral is warranted if the athlete is not responding to treatment or if heatstroke is suspected.
Treatment and Return to Participation
Treating thermoregulatory problems in patients with a spinal cord disability is similar to that for the general population. For hyperthermia, the patient is moved to a shaded or cooled area, clothing is loosened, equipment is removed, oral fluids are administered, and cooling is accomplished with cold water. Intravenous fluids are administered if the patient is not coherent. If heatstroke is suspected, emergency measures to reduce the patient’s temperature (e.g., sponge application of cool water, fanning the body with a towel) are performed first; then the individual must be transported to an advanced emergency care facility. Although immersion in an ice bath has been recommended, this treatment should be used with caution for individuals with SCI, especially those with a complete, high level of lesion: Their thermoregulatory system is impaired, and cooling may occur too rapidly. To date, research in this area for individuals with SCI is incomplete. Therefore, the patient’s physician should discuss indications and contraindications before the patient exercises in the heat.
Treating hypothermia involves administering warm fluids, transporting the patient to a warm environment, and removing wet clothing immediately and replacing it with warm, dry clothing. Heat applied to areas without sensation is contraindicated, so use of heating pads or hot water bottles on paralyzed areas should be avoided.
The National Athletic Trainers’ Association established an Inter-Association Task Force that created a statement on exertional heat illness containing return-to-activity guidelines. In general, these guidelines include physician clearance and gradual and monitored return to activity, and they may be used with patients with SCI as well.
Prevention
Heat-related illnesses are entirely preventable. Hyperthermia can be prevented by ensuring availability of proper hydration and rehydration techniques, appropriately adapting to environmental conditions, wearing appropriate clothing, and screening for a prior history of heat-related illnesses. Individuals who use a wheelchair should attach to the chair a water bottle for drinking and a spray bottle for surface cooling. A tented area adjacent to the competition should be established to provide ready access to shade. Medications should be monitored, because some nutritional supplements and prescription, over-the-counter, and recreational drugs can adversely affect heat production and heat loss. The risk of heat illness is much greater for individuals who use these agents, so it stands to reason that some medications could influence similar mechanisms in individuals with SCI. Certain medications may also predispose individuals to temperature regulation problems in the cold.
Prevention of hypothermia includes encouraging individuals to drink plenty of fluids, warm up properly, wear adequate layers of clothing, change wet clothing immediately after exercise, and wear a hat. Athletic trainers should screen participants for a history of hypothermia.
Special Concerns in the Adolescent and Mature Individual
Athletic trainers should also closely monitor youth or master-level athletes for thermoregulatory issues.30 Children tend to absorb more heat from their surroundings, have a lower sweating capacity, and produce more metabolic heat per mass unit than adults. Therefore, exercise time and intensity are reduced when environmental conditions are extreme. In addition, athletic trainers should make sure that children have 10 to 14 d of acclimatization. Older adults may have decreased fitness levels, decreased lean body mass, and chronic diseases and may use prescription medications, all of which may affect their reaction to the environment. Athletic trainers should check for fitness, acclimatization, and frequent fluid intake, and they should consult with the patient’s physician about medications.
SHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- Women in sport and sport marketing
- Sport’s role in the climate crisis
- What international competencies do sport managers need?
- Using artificial intelligence in athletic training
- Using the evidence pyramid to assess athletic training research
- How can athletic trainers ask a clinically relevant question using PICO?


