The Achilles tendon and its pathologies
This is an excerpt from Biomechanics of Injury-3rd Edition by Ronald F Zernicke,Steven P Broglio,William C Whiting.
Calcaneal Tendon Pathologies
Ever since the Greek warrior Achilles was felled by an arrow judiciously aimed at his unprotected heel, the calcaneal region has been associated with susceptibility to injury.
The calcaneal (Achilles) tendon, the largest and strongest tendon in the body, is formed by merging of the distal tendons of the gastrocnemius and soleus about 5 to 6 cm proximal to its insertion site on the posterior surface of calcaneus. At the insertion site, tendon width varies from 1.2 to 2.5 cm. Approximately 12 to 15 cm proximal to the insertion, the calcaneal tendon begins to spiral, twisting about 90° as it approaches its calcaneal insertion (Schepsis et al. 2002).
Frequent and repeated loading of the calcaneal tendon predisposes it to overuse pathologies, most commonly peritenonitis (inflammation of the peritenon), insertional disturbances (e.g., bursitis or insertion tendinitis), myotendinous junction injury, or tendinopathies (Kvist 1994).
The calcaneal tendon transmits substantial loads from the triceps surae muscle group (gastrocnemius and soleus) to its attachment on the posterior calcaneus. A sample of studies confirms the high loads transmitted by the calcaneal tendon:
- Burdett (1982), using a biomechanical model, estimated peak calcaneal tendon forces ranging from 5.3 to 10.0 times body weight during the stance phase of running.
- Fukashiro and colleagues (1995), using an implanted tendon force transducer, reported peak calcaneal tendon force of 2233 N (502 lb) in the squat jump, 1895 N (426 lb) in the countermovement jump, and 3786 N (851 lb) in hopping.
- Giddings and colleagues (2000), using experimental data and a quantitative model, predicted maximal calcaneal tendon force 3.9 times body weight for walking and 7.7 times body weight for running, with the peak loads at 70% of the stance phase for walking and 60% of stance for running.
- Bogey and colleagues (2005), using an electromyograph-to-force processing technique, estimated peak calcaneal tendon force of 2.9 kN (652 lb) during gait.
- Pourcelot and colleagues (2005), using a noninvasive ultrasonic technique, found peak calcaneal tendon forces of about 850 N (191 lb) during the stance phase of walking.
- Revak and colleagues (2017), using kinematic and force plate measures, reported lower calcaneal tendon loading in bilateral and seated heel-raising and -lowering exercises when compared to unilateral and standing conditions.
- Gheidi and colleagues (2018) using a musculoskeletal model, compared calcaneal tendon loading during weight-bearing exercises, with highest peak force (6.68 times body weight) in a unilateral jump landing, and lowest peak force (0.77 times body weight) in a squat exercise.
Although the calcaneal tendon clearly is subjected to high magnitude loads across a spectrum of activities, Komi and colleagues (1992) suggested that the loading rate may be more clinically relevant than the loading magnitude.
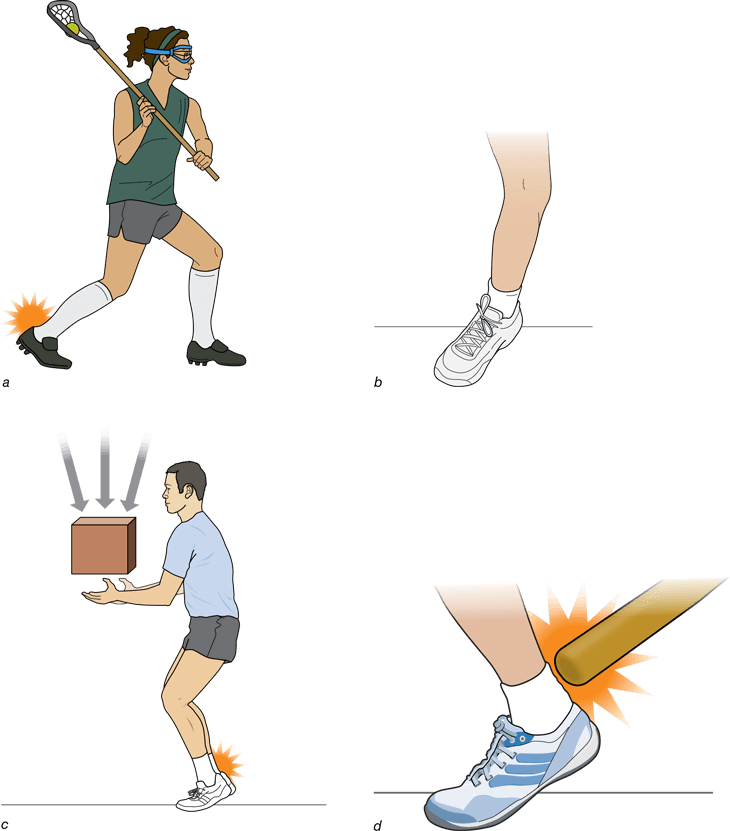
Four primary mechanisms have been implicated in calcaneal tendon rupture (Mahan and Carter 1992; figure 6.44): (1) sudden dorsiflexion of a plantarflexed foot (e.g., a lacrosse player in the act of throwing), (2) pushing off the weight-bearing foot while extending the ipsilateral knee joint (e.g., a basketball player executing a rapid change of direction), (3) sudden excess tension on an already taut tendon (e.g., catching a heavy weight), and (4) a taut tendon struck by a blunt object (e.g., softball bat). These mechanisms suggest, and epidemiological evidence confirms, that most calcaneal tendon ruptures are unilateral. Although rare, bilateral calcaneal tendon ruptures have been reported (Garneti et al. 2005).
The cause of calcaneal tendinopathies is multifactorial; contributing factors include training errors, running terrain, malalignments (e.g., combined flat foot and excessive pronation) and biomechanical faults, improper footwear, trauma, age, sex (men are at 5-6 times greater risk of rupture than women), anthropometrics, environment, and psychomotor factors. The tendon also may be weakened, and thus put at even greater risk, by systemic diseases, steroids, and fluoroquinolone antibiotics (Casparian et al. 2000; Maffulli and Wong 2003; Vanek et al. 2003). Nonuniform tendon stresses attributable to individual muscle contributions may also contribute to injury risk (Arndt et al. 1998).
Tendon degeneration may eventually lead to complete tendon rupture. Calcaneal tendon ruptures typically happen in sedentary, 30- to 40-year-old men who suddenly exert themselves in a sporting task that involves running, jumping, or rapid change of direction (Järvinen et al. 2001; Schepsis et al. 2002; Yinger et al. 2002). In many instances these spontaneous tendon ruptures seem to “just happen.” Postinjury assessment, however, shows evidence of degeneration in the ruptured tendon. Tendon rupture thus often occurs secondary to degenerative processes rather than as a spontaneous primary injury.
Calcaneal tendon rupture usually occurs about 2 to 6 cm proximal to the calcaneal insertion in a region known to be hypovascular. This fact, combined with decreased blood flow associated with age, helps explain the frequency of rupture in middle-aged people. The calcaneal tendon has a poor blood supply that previously was thought not to vary along its length (Ahmed et al. 1998). A study using a novel method, however, reported an avascular region close to the calcaneal insertion site and regional differences in vascular density along the tendon length (Zantop et al. 2003). The middle part of the calcaneal tendon had a much lower vascular density (28.2 vessels/cm2) than either the proximal part (73.4 vessels/cm2) or the distal part (56.6 vessels/cm2). The authors identified this reduced vascularization (and resulting hypoxia) as a predisposing factor for calcaneal tendon degeneration and eventual rupture. In addition, the distal portion of the Achilles tendon is at greater risk of rupture due to its smaller cross-sectional area distally compared to proximally (Reeves and Cooper 2017).
As a side note of interest, there may be a relation between blood type and increased incidence of tendon rupture. Persons with type O blood seem to be more likely to suffer from tendon rupture in general (Jόzsa et al. 1989) and calcaneal tendon rupture in particular (Kujala et al. 1992) compared with people who have other blood types, suggesting a genetic link between one’s ABO blood group and the molecular structure of tendon tissue. Another study, however, found no significant relation between the proportions of ABO blood groups and Achilles tendon rupture (Maffulli et al. 2000). Maffulli and colleagues concluded that the association between blood group and tendon rupture may be attributable to differences in blood group distribution in genetically segregated populations. Genetic factors also play a role in predisposition to calcaneal tendon rupture (Ribbans and Collins 2013).
Predisposition to rupture also may be affected by collagen type. Eriksen and colleagues (2002) found type III collagen accumulation at the rupture site, likely attributable to microtrauma and healing events. Similar results of higher type III collagen at calcaneal tendon rupture sites have been reported (Pajala et al. 2009). Increased type III collagen content may contribute to lower tendon tensile strength and enhanced rupture risk.
In summary, the theoretical explanations for Achilles tendon ruptures and other chronic pathology suggest a sequence of events that is initiated with an intrinsic tendon pathology associated with disuse, age-related tendon change, and hypovascularity, resulting in localized degeneration and tendon weakening. This decreases the tendon’s threshold to rupture. The precise proprioceptive and pathomechanical position and load that causes the injury remains obscure. It is probably a complex equation of neuromuscular control and endocrine factors that result in the Achilles tendon rupture. (Yinger et al. 2002, p. 234)
More Excerpts From Biomechanics of Injury-3rd EditionSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?
- How do hormones affect muscles?
- Machine learning: The cornerstone of data-driven decision making for sport organizations
- Examples of how systematic reviews and meta-analyses are used in sport


