Identifying Exercise-Induced Bronchospasm
This is an excerpt from Medical Conditions in the Athlete 3rd Edition With Web Study Guide by Katie Walsh Flanagan,Micki Cuppett.
The terms exercise-induced asthma (EIA) and exercise-induced bronchoconstriction (EIB) are often used interchangeably, but EIB specifically denotes the reduction in lung function that occurs after a standardized exercise test (Carver 2009). More recently, the term exercise-induced bronchoconstriction has been introduced as actual spasm of the airways does not always occur. Some clinicians use EIA to describe individuals with known asthma who have bronchoconstriction during exercise. However, some use EIA to describe patients who have bronchoconstriction only during exercise, and they use EIB to describe patients with asthma who have bronchoconstriction with exercise. Generally, EIB is used to indicate bronchospasm with decreased pulmonary function testing following exercise, and EIA is used to indicate those patients with asthma difficulties associated with exercise.
Symptoms of EIB usually occur 10 to 15 min after the onset of strenuous exercise and are defined by a fall in FEV1 of 15% or more during exercise spirometry. EIB is more common in winter sport athletes who compete in cold ambient temperatures (Carey, Aase, and Pliego 2010).
Signs and Symptoms
EIB should be suspected in any athlete who complains of shortness of breath, dyspnea, cough, chest congestion, or tightness with exertion. These symptoms usually occur during strenuous exercise and peak about 5 to 10 min after exercise (Hull 2012; Krafczyk and Asplund 2011; Simpson, Romer, and Kippelen 2015). Other subtle clues might be a dry cough that develops after practice or exercise (i.e., locker-room cough) or simply unusual fatigue compared with similarly trained athletes. Athletes will often complain that they feel out of shape despite regular training. Self-reported symptoms have been shown to be poor predictors of EIB because other conditions can cause similar symptoms. Symptoms alone should not be used to diagnose EIB.
In athletes suspected of having EIB, other etiologies, such as acute sinusitis, otitis media (middle ear infection), bronchitis, or even pneumonia, need to be excluded, particularly in the context of other constitutional symptoms, such as fever, chills, or night sweats. If fatigue is the only presenting symptom, deconditioning may also be a cause. In addition, environmental allergies can account for many of the nonspecific symptoms that mimic EIB (Backer 2010; Hull et al. 2012; Stack and Hakemi 2011). More serious cardiac causes, such as arrhythmias and pericarditis, might also need to be excluded. Another important differential is exercise-induced laryngeal obstruction (EILO), where the wheezing and dyspnea are caused by transient obstruction of the upper airways during exercise (Nielsen 2013; Backer 2010).
Referral and Diagnostic Tests
The physical examination is usually normal. Some athletes with EIB may experience symptoms that develop several hours after exercise. This late-phase response is due to the activity of inflammatory mediators. Most commonly, a bronchial provocation challenge is used to determine the diagnosis of EIB (Parsons et al. 2011; Hayden et al. 2011; Morris 2010). Figure 7.9 shows a decision tree commonly used for the diagnosis of EIB. Alternatively, many physicians choose to just evaluate the patient's response to an empirical trial of a ß-agonist medication before exercise.
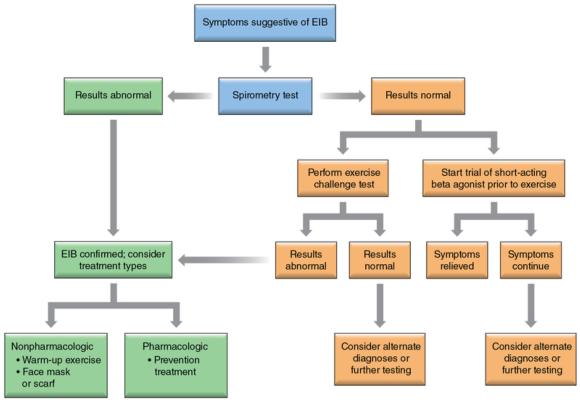
Decision tree for the diagnosis of exercise-induced bronchoconstriction (EIB).
Treatment and Return to Participation
The treatment of choice in EIB is an inhaled ß2-agonist from a metered-dose inhaler (e.g., albuterol) taken 15 to 30 min before the onset of exercise. An athlete who has asthma symptoms outside the exercise setting or who is using a ß2-agonist more than three times per week should be treated with a regular inhaled corticosteroid. Here is how to properly use an inhaler:
- Remove dust cap and shake the inhaler system before each use.
- Inspect mouthpiece for contamination or foreign objects.
- Breathe out through the mouth, exhaling as completely as possible.
- Hold the inhaler system upright with mouthpiece in mouth and lips closed tightly around mouthpiece.
- Breathe in slowly while pressing down on the metal cartridge.
- Hold breath as long as possible.
- Release pressure while still holding breath.
- Remove mouthpiece.
- Wait for the container to repressurize, shake, and then repeat steps 3 through 8 when more than one inhalation is prescribed.
- Rinse mouth with water after prescribed number of inhalations.
- Clean the inhaler system every few days by removing metal cartridge and rinsing the plastic inhaler and cap with running warm water. Replace cartridge and cap.
Emerging studies show promise using long-acting ß2-agonists such as salmeterol and leukotriene inhibitors such as montelukast (Singulair) (Parsons 2010). Other nonpharmacological strategies include pre - warm-up bursts of physical activity at 80% to 90% of the individual's maximal workload to induce a refractory period that lasts up to 3 h after the initial attack of EIB (Hull et al. 2012; Millward et al. 2009; Boulet, Hancox, and Fitch 2010). Strategies to humidify inspired air and dietary interventions may also prove to be beneficial (Carey, Aase, and Pliego 2010; Bussotti, Di Marco, and Marchese 2014).
For an athlete experiencing a severe asthma attack or when an inhaler is ineffective, a nebulizer may be used. A nebulizer, also known as an atomizer, is a machine that vaporizes liquid medication into a fine mist to be inhaled into the lungs via a mouthpiece or mask. Although studies have shown that both inhalers and nebulizers tend to be equally effective in delivering medications, nebulizers are preferred for use in more serious rescue situations when the patient is experiencing a severe asthma attack. Nebulizers can administer a higher dose of medication, but inhalers are easier to use, preferred for their portability and low cost, and good for everyday use. Medications typically administered with a nebulizer include albuterol and ipratropium (Atrovent).
Athletes with controlled EIB need not be excluded or discouraged from participating in sports. Effective strategies, both pharmacological and nonpharmacological, exist that can allow an athlete to compete even at an elite level.
Learn more about Medical Conditions in the Athlete, Third Edition.
More Excerpts From Medical Conditions in the Athlete 3rd Edition With Web Study GuideSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- Using double inclinometers to assess cervical flexion
- Trunk flexion manual muscle testing
- Using a goniometer to assess shoulder horizontal adduction
- Assessing shoulder flexion with manual muscle testing
- Sample mental health lesson plan of a skills-based approach
- Sample assessment worksheet for the skill of accessing valid and reliable resources


