Getting the most from diabetes technologies
This is an excerpt from Athlete’s Guide to Diabetes, The by Sheri Colberg-Ochs.
Technology and software related to diabetes and health management are advancing faster than most people can keep up with. Every day a new app seems to come out to keep track of something, be it your blood glucose levels, insulin on board, and carbohydrate counting or your calories, daily steps, and fitness goals. In the diabetes world, the latest management technologies guide people in making more informed and effective regimen change decisions—the most important of which are integrated systems that can take charge of the decision making by combining delivery of insulin via pumps, continuous glucose monitoring (CGM), and a control system with potential artificial intelligence(AI) capabilities. Next down the pike is integration of wearable technologies, which can add information related to heart rate and more. More improvements will make AI even more capable of “learning” and updating algorithms to match the changes and patterns in your metabolic state.
Given the challenges of exercising with diabetes, the latest technologies can be beneficial for managing your blood glucose and maximizing the benefits of physical activity. Insulin pumps (covered fully in chapter 3) offer a more fine-tuned ability to regulate basal insulin levels and bolus doses. Blood glucose meters give immediate feedback on where your glucose is starting and how you are responding to an activity. The CGM devices provide an added level of safety by offering the opportunity for improved decision making in real-time and retrospectively. Closed-loop systems that integrate a pump and CGM manage the decision making for you; they can potentially improve your blood glucose management before and during exercise and allow you to avoid any unwanted rises and falls in your blood glucose after workouts. All forms of technology have inherent drawbacks and limitations, but you can overcome most of their issues with planning and knowledge.
Blood Glucose Meters (and Their Precursors)
If you began your journey with diabetes after the advent of home blood glucose meters, consider yourself lucky. Back in 1968 when I began my life with diabetes, no one had blood glucose meters to use for self-monitoring, much less target blood glucose ranges for exercise. All we had were urine tests, which measured the excess glucose and ketones in urine. You would pee in a cup, then put 5 drops of urine with 10 drops of water into a test tube with a tablet. The test tube mixture changed color in a range from cool blue (no glucose) to flaming orange (4+glucose). It did not give you the foggiest idea of what your blood glucose was doing right then; it only told you whether you had been higher than optimal a few hours before. In other words, you could be shaking with the symptoms of a low while watching your urine turn bright orange, the indication of being very high. The ketone test strips merely confirmed what you already knew: you had some ketones in your urine (and therefore your blood) most of the time because the diabetes management tools were lacking.
The next generation of urine test strips eliminated the precise drops and test tubes, but they were not necessarily an improvement. After dipping the test strip in your urine, you had to match the color of the strip to a chart on the side of a bottle. Your six choices ranged from light blue to dark brown, corresponding to negative (0), 100, 250, 500, 1,000, and 2,000 mg/dL or more. This still did not give you a clue about the level of your blood glucose.
The blood glucose test strips of the early 1980s would only estimate your blood glucose within maybe 40 mg/dL (2.2 mmol/L), assuming your glucose was under 200 mg/dL (11.1 mmol/L). Over that range, from one color block to the next, the number jumped up by 100 to 200 mg/dL or more. In other words, blood glucose strips still were not remotely precise enough to allow anyone to safely make regimen changes.
Relatively small and affordable blood glucose meters did not become widely available to individuals until the mid-1980s. I got my first one in 1986 after I had already been living with type 1 diabetes for 18 years. My first meter still had significant potential for user error because you had to blot the blood off the strip halfway through the 2-minute testing period. Even with access to reasonably accurate blood glucose measurements for the first time, we all experienced a steep learning curve while figuring out what to do with our food or insulin in response to the readings.
The moral of this story is that we have come a long way with diabetes technology, even if all you use currently is a blood glucose meter that gives you feedback in only 5 seconds. Appreciate having the ability to check what your blood glucose is doing at any given moment and learn to use that vital information to expertly manipulate your medication doses and diet.
With access to a blood glucose meter, you have the primary tool you need to manage your diabetes effectively, especially with exercise as an added variable. Check as frequently as you need to, with the goal of avoiding both lows and highs.
Even if you do not normally get low during exercise, checking frequently is still advisable, especially before you start and after you finish working out. Once you learn your usual responses to activities, you can usually anticipate how to react to keep your blood glucose in an optimal range to perform well.
Continuous Glucose Monitors
In the past decade or so, a number of continuous glucose monitoring (CGM) devices have received approval from the U.S. Food and Drug Administration (FDA), the European Commission, and across the world. To date, all of them are still invasive: they require that you place and keep a probe of some sort under your skin to get readings. While many innovators are working on noninvasive CGM devices, none have been approved or are available yet for use. At least one company (Senseonics) has FDA approval for an implantable CGM device called Eversense, which lasts for 3 months at a time, and they are seeking approval for up to 180 days. (I have heard that their sensors go in easily during an office visit, but they are more difficult to remove after 90 or 180 days. That is not surprising: that time span is more than sufficient for your body to develop an inflammation and grow new tissue around a foreign object embedded in your skin.)
These monitors by themselves only give you information—much like a blood glucose meter does—but you still have to check the readings and make regimen adjustments yourself. However, getting feedback in real-time or at least every 1 to 5 minutes, 24 hours a day, can be extremely useful when you are trying to learn your patterns, see the trends, or keep your blood glucose in a tighter range with less hypoglycemia. The accuracy of these meters has been improving over time, but they are all still limited by their physiological methods: there is a lag of at least 6 to 20 minutes between the glucose they measure (in interstitialspaces between cells in the skin) and your actual blood glucose. This lag can be even greater during times when your blood glucose levels are often changing rapidly, such as after a meal or during exercise.
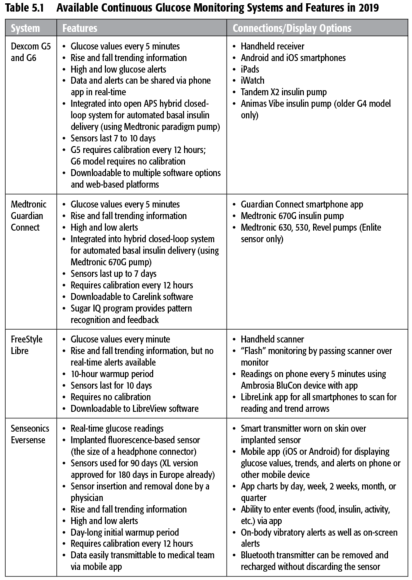
The CGM devices and models approved and available in the United States as of the publication of this book are shown in table 5.1. “Flash” glucose monitoring (as offered by the FreeStyle Libre device) is a recent innovation, possessing some but not all features of traditional CGM. Flash monitors can provide instantaneous glucose values and recent trends, but they lack the alerts for lows and highs.
Insurance reimbursement also has become more reasonable since CGM devices were first introduced over a decade ago. (I paid $35 out of pocket for each 3-day sensor for the first-generation Dexcom CGM I tried.) Currently, at least one model is covered by Medicare for anyone with type 1 diabetes age 65 and over. Studies have shown that people with type 2 diabetes—especially those using insulin—can also benefit from using CGM, but coverage for them has been an even harder sell to insurance companies so far. In any case, the number of model choices has declined recently, and their cost is still prohibitive for people who lack the insurance coverage.
What's more, CGM technology is not infallible. As I have noted, a major drawback of CGM devices used during exercise is that their glucose readings are not fully real-time because they measure glucose levels in your skin rather than in your blood, and it takes some time for glucose to move between these two parts of your body. Also, CGM users may have problems getting the device to stay put, similar to the issues experienced by pump users with their infusion sites. (Refer back to table 3.2 for solutions on resolving adhesion issues and to the list of strategies used by athletes in chapter 12; most of the tactics used to secure a pump infusion site will also work for CGM devices.) Other reported challenges include variable sensor accuracy, variable performance between sensors, breakage of sensor filaments, transportation of the sensor display, and inability to calibrate CGM during exercise. (If you have the option, you may want to use an integrated watch to display your values.) Although technical failures during exercise are possible even with the newer versions of these monitors, CGM is still the wave of the future when it comes to monitoring and managing blood glucose.
Exercisers have reported a compression effect when wearing the CGM sensor in areas underneath compression shorts, resulting in a greater lag time in readings due to reduced blood flow to areas with compressed skin. This can also happen when you lie directly on the sensors.
If you have access to CGM, you may be able to use either traditional CGM or Flash monitors to enhance your exercise experience in a variety of ways.
- Seeing your glucose values before exercise tells you whether you are likely to need extra carbohydrates, insulin reductions, or an insulin bolus.
- Knowing your glucose trends before you start to work out can also help you make more informed decisions about any necessary changes in your food or medications.
- High and low alerts during and after exercise can help you avoid dangerous glucose extremes, particularly if you set your alerts at preemptive or conservative levels.
- Reviewing your trend graph reports after working out can show you the patterns of your exercise highs and lows, particularly if you use event markers or workout logs.
Many exercisers swear by their CGM devices and do not want to have to live without them (and hopefully they will not ever have to). But if you do not have access to CGM due to lack of insurance coverage, availability in your country, or other reasons, do not despair—you can still learn your glucose patterns by using frequent checks with a blood glucose meter, as most of us have done. In general, most athletes using CGM have found that observing their glucose trends (shown by up, steady, or down arrows) can be helpful during exercise, even when the readings lag behind actual blood glucose or are sometimes inaccurate.
SHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- How do I integrate nutrition education into PE?
- How does the support of friends and family influence physical activity?
- What makes the Physical Best approach unique?
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?


