Focusing your examination approach
This is an excerpt from Orthopedic Clinical Examination With Web Resource by Michael P Reiman.
Broad to Narrow or Funnel Examination Focus
The entire diagnostic process entails each component described in this text. This examination focus or sequence will be referred to as broad to narrow or the funnel approach as advocated by the author and colleagues. The clinician generates a differential diagnosis for each client based on the history (client interview), observation, triage, motion, muscle performance, special tests, palpation, and physical performance measures (figure 4.1). Based on the probability of a particular diagnosis to exist, the findings of each of these components will make shifts in posttest probability based on their diagnostic accuracy (SN, SP, likelihood ratios). Utilizing only one component as the gold standard from which the diagnosis is made is inappropriate clinical practice.
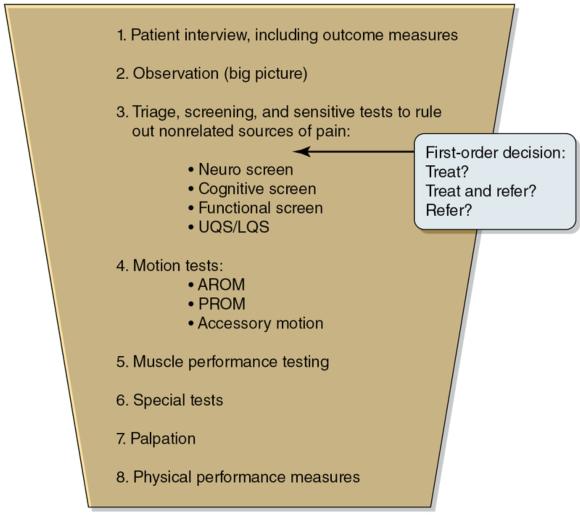
Funnel approach of the examination process.
© Michael Reiman
This approach, while comprehensive, is also systematic; it moves from broad to narrow in its approach from the beginning to the end of the examination process. The intent is to start the examination process as comprehensively as possible, including all potential diagnoses. As a result of each systematic step in the examination process, the clinician should narrow down the differential diagnosis list as far as possible. Additionally, the broad-to-narrow approach of the examination is in the sense of moving from less to more isolated examination procedures. For example, in the client interview, the clinician asks broad, open-ended questions that are likely to include multiple potential diagnoses. As the examination continues, the examination process becomes more focused. This is particularly the case after the section for triage or screening and sensitive tests, which is intended to rule out not only the potential for red flags or nonmusculoskeletal disease processes but also potential pain generators in other joints, as well as other potential diagnoses common to the pain-generating joints.
Integration of Funnel Examination Approach
A systematic approach to using findings (especially those from special tests) reporting SN and SP is suggested in figure 4.2. The use of tests of high SN and low -LR is suggested early in the examination (Triage and Sensitive Tests), with red flags first ruled out. Once it is determined that the client is appropriate for examination or treatment, the clinician continues through additional examination components (e.g., motion tests, muscle performance testing, special tests). Particular emphasis is on motion testing and muscle performance testing to delineate if the client's actual symptoms are reproduced. Additionally, special tests (and possibly imaging) of high SP are helpful to rule in pathology of the determined pain-generating joint(s). Again, caution should be taken when using special tests for diagnosis. Figure 4.2 shows a systematic approach for integrating diagnostic accuracy findings of both high SN (early in the examination - triage and screening) and high SP (later in the examination - special tests - for determination of ruling in pathology). The suggestions for ideal and good diagnostic accuracy values are again provided here.
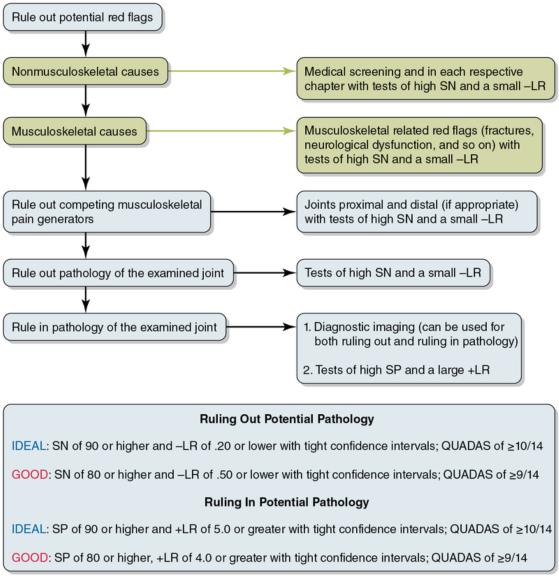
Algorithm approach for use of special tests or findings reporting SN and SP. SN = sensitivity; SP = specificity; +LR = positive likelihood ratio; -LR = negative likelihood ratio
© Michael Reiman
The Examination Continuum
The examination of a client should also be recognized as an assessment along a continuum (figure 4.3). Many examination procedures described, including those in this text, are on the isolated examination side of the continuum (e.g., ROM, muscle performance, radiology findings, special tests). Integrated examination would include measures more applicable to daily tasks, such as sport- and work-related activities (e.g., function). These measures might include administering the physical performance measures section of this text (see chapter 12), as well as simply assessing the client's quality and big-picture quantity assessment of their daily tasks, work tasks, and sports tasks.

The examination continuum.
© Michael Reiman
Note that clients likely will move back and forth along this continuum at different points in their rehabilitation process. For example, a client progressing appropriately along post knee injury, but who still has pain with jumping, may require a reassessment where they enter the continuum with a jumping assessment first (toward the integrated side of the continuum). This will help the clinician determine the potential limitation or pain generator from which to then focus the isolated examinations, as described previously.
Learn more about Orthopedic Clinical Examination.
More Excerpts From Orthopedic Clinical Examination With Web ResourceSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- How do I integrate nutrition education into PE?
- How does the support of friends and family influence physical activity?
- What makes the Physical Best approach unique?
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?


