Evaluation of the Skin
This is an excerpt from Medical Conditions in the Physically Active 4th Edition With HKPropel Access by Katie Walsh Flanagan,Micki Cuppett.
The goal of a skin examination by the health care provider is to identify, or attempt to identify, unknown skin lesions to determine the need for referral, need for treatment, or activity status (i.e., to allow participation or to withhold from participation), and to prevent transmission among athletes. New or previously undiagnosed lesions must be diagnosed and treated or, at minimum, carefully watched for changes. A history and a visual inspection can be very revealing; exactly how revealing depends on the patient’s history, the quality of the visual inspection, and the patient’s willingness to be truthful in either reporting or trying to hide a skin lesion. The athletic trainer should be suspicious of an athlete-patient wearing a wrap or a bandage that the athletic trainer did not apply. When asking the patient to disrobe for a skin inspection, all tape, wraps, and bandages should be removed. Wrestlers have been known to self-abrade (e.g., using sandpaper) or to apply caustic chemicals (e.g., bleach) to skin lesions to hide or remove the infection.
When working with athletes whose sports put them in close skin-to-skin contact, such as wrestlers, a skin examination should be performed often enough to detect newly forming and potentially contagious lesions early enough to initiate treatment and to prevent transmission to others. Weekly skin examinations are considered the norm; however, when the possibility of an active outbreak exists, they should be performed often enough to detect new lesions immediately, thereby shortening the course of the outbreak among team or family members. For athletes, specific league rules may require that full-body skin examinations be performed at specified intervals; however, compliance with league rules should be viewed by the athletic trainer only as the minimal standard, especially when more frequent inspections are warranted.
A skin inspection should be conducted in a well-lit room that provides a private, respectful environment. For full-body examination, males should be wearing only shorts, while females should be wearing shorts and a sports bra or swimsuit top. Whenever possible, a health care provider of the same sex should conduct the examination. Begin the examination by obtaining a patient history. Ask if the patient has any skin problems to report and if they have felt ill or have nausea, fever, body aches, or fatigue. These symptoms may be especially indicative of viral or bacterial infections. The visual inspection is conducted with the patient standing erect, feet shoulder-width apart, arms abducted to 90°, and palms forward with hands open. Avoid touching the patient whenever possible; however, this may be unavoidable when examining specific body parts, especially the scalp. If contact is necessary, athletic trainers should wear gloves and should change them and disinfect their hands between patients to avoid cross-contamination. Begin a systematic inspection of the patient, including all aspects of the upper and lower extremities and the torso, including the axilla, neck, face, and scalp. The scalp is especially important because hair may conceal active infections. Patients should be able to adjust their neck and move their hair to facilitate the inspection, but the on-site health care provider may have to physically part the hair to visualize the scalp.
The athletic trainer should look for any abnormalities and should note specifically the pattern, color, and location of all lesions:
- Pattern: Does the lesion appear scratched, raised, depressed, or in groups or clusters, and is it bullous, moist, dry or crusted, or draining fluid?
- Color: What is the color of the lesion, the surrounding tissue, and the fluid or crust, and is the color uniform with well-defined borders and symmetry?
- Location: Is the lesion above or below the hairline on the scalp, on or near the genitals, or on or near the mouth?
The athletic trainer is usually the first clinician to evaluate a dermatological lesion on a patient. A lesion is synonymous with abnormal tissue. The key is to look for tissue abnormal to the surrounding area. A freckle is also one form of a lesion. Lesions are typically in the very early stages of development and can be difficult to differentiate without microscopic or laboratory testing. Because these types of diagnostic procedures are beyond the scope of many health care providers, the athletic trainer must use sound clinical judgment when determining the appropriate course of action for patients with dermatological conditions.
When referral to a medical doctor for evaluation and treatment is necessary, the health care provider must understand the patient’s signs and symptoms and be able to effectively describe findings to the physician using dermatographical nomenclature. The terminology used to describe the appearance of a skin lesion or condition is very specific (figure 16.3). The athletic trainer must have the knowledge and resources necessary to make these distinctions. It is much easier and more efficient to describe the lesion as a fissure rather than as a “linear loss of epidermis and dermis with sharp, defined borders.” The clinician must also understand that these terms are important to the description and are not a specific diagnosis.
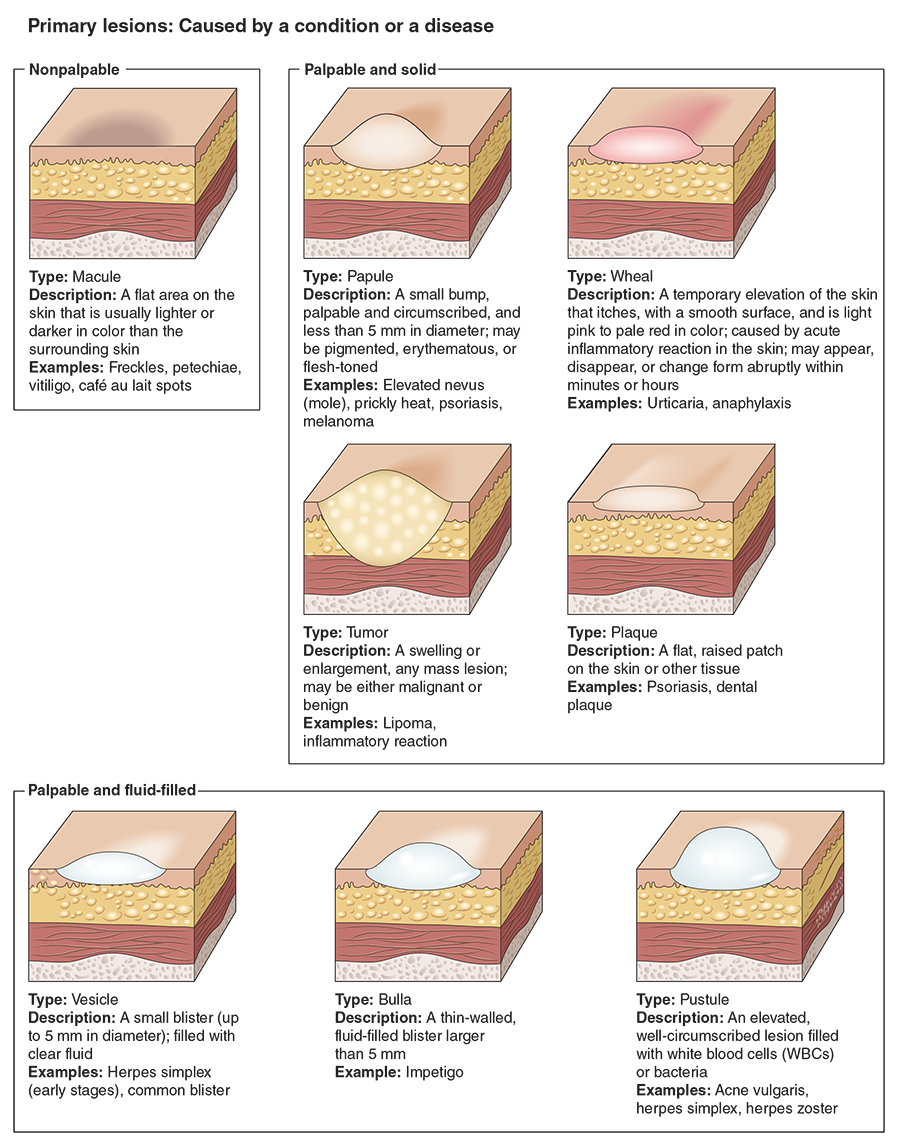
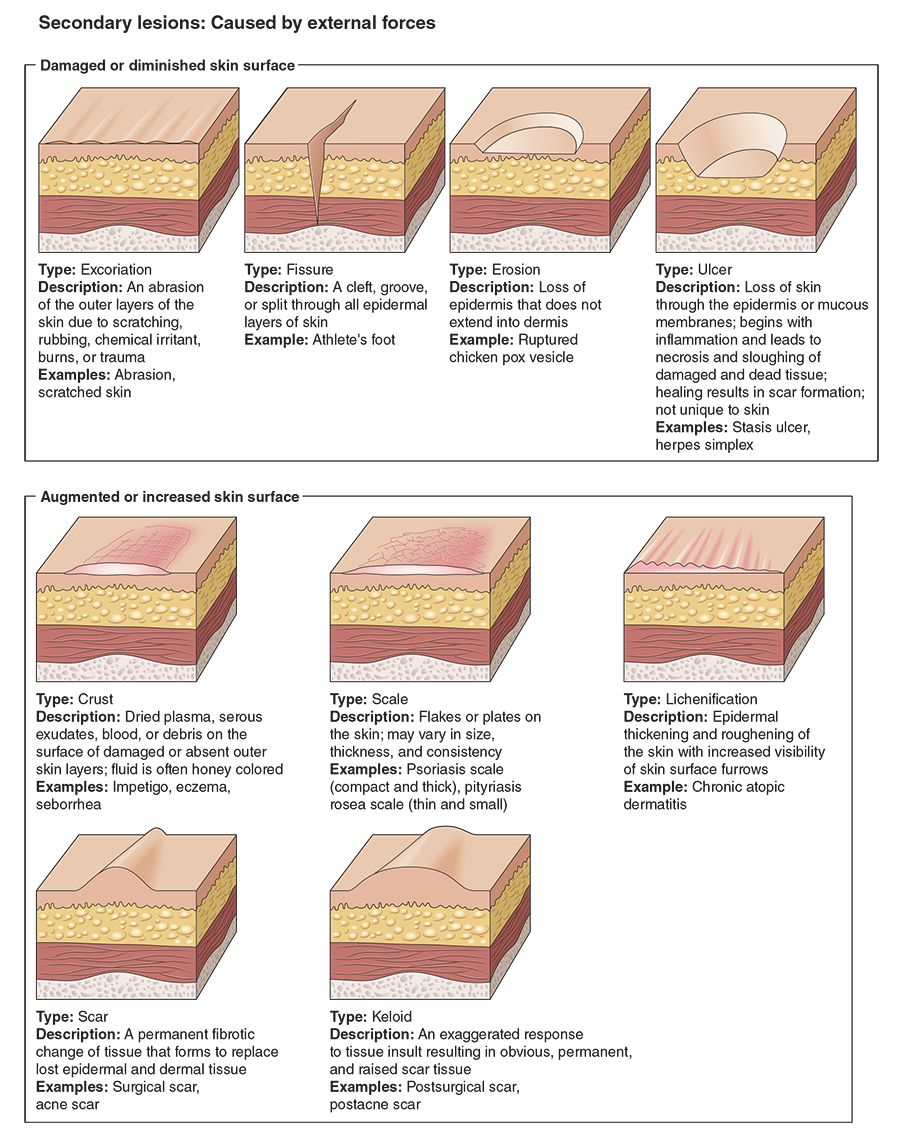
Dermatitis, for example, is an inflammation of the skin or dermal layers and can result from a variety of dermatological conditions with various causes. The term dermatitis merely indicates a general inflammation of the skin, whereas contact dermatitis indicates an inflammation of the skin caused by direct contact with a specific allergen, and actinic dermatitis indicates inflammation of the skin from exposure to sunlight or another irritating light source.
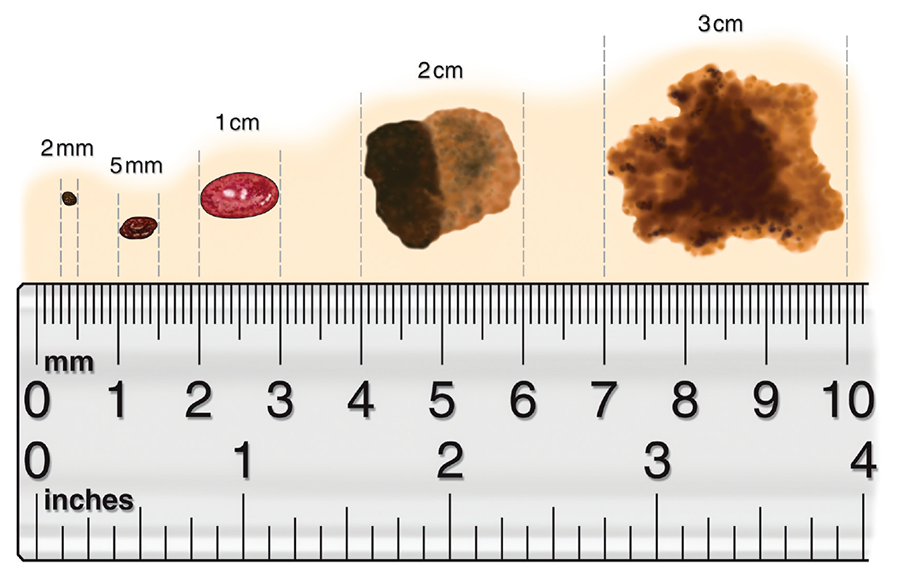
Another way to describe dermatological conditions is by referencing the area of skin affected. Most physicians use millimeters to describe the width or breadth of a condition, but centimeters are used for larger surface areas. As a point of reference, 1 in. is equal to 25.40 mm or 2.54 cm (figure 16.4).
More Excerpts From Medical Conditions in the Physically Active 4th Edition With HKPropel Access
SHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- Women in sport and sport marketing
- Sport’s role in the climate crisis
- What international competencies do sport managers need?
- Using artificial intelligence in athletic training
- Using the evidence pyramid to assess athletic training research
- How can athletic trainers ask a clinically relevant question using PICO?


