Electrolyte Losses and Replacement During Exercise
This is an excerpt from Sport Nutrition 4th Edition With HKPropel Access by Asker Jeukendrup,Michael Gleeson.
Electrolytes are minerals that dissolve in water into their individual positively or negatively charged ions. Sodium (Na+) and chloride (Cl−) are the two electrolytes lost in the largest quantities through sweating (losses of other electrolytes such as magnesium and zinc are much smaller and are discussed in chapter 10), but sodium losses are also regulated in response to the balance of dietary sodium intake and additional recent sodium losses in urine.
The addition of sodium to drinks in the resting state can improve the amount of that fluid retained, rather than lost through urination. The inclusion of some sodium in drinks that are consumed during exercise improves their flavor and tends to encourage consumption, which can be useful in terms of preventing excessive fluid losses during exercise, and it helps to maintain blood osmolality and reduce the risk of developing hyponatremia (a fall in the plasma sodium concentration). There is some controversy about the need to replace sodium during exercise in order to maintain performance or prevent or delay the onset of muscle cramp, so let us now consider these issues.
Is Sodium Replacement During Exercise Necessary?
In some sports it appears to be popular to ingest salt tablets during prolonged competition with the presumed aim of restoring salt losses in sweat to improve performance and reduce the risk of developing muscle cramping. Most sports drinks also contain some sodium (typically 20-25 mmol/L), and this is often claimed to offset sodium losses in sweat. But does sodium (salt) ingestion during exercise actually improve performance? Surprisingly, there are very few studies on this topic, and a review by McCubbin and Costa (2018) concluded that on the basis of the results of five available relevant studies (Cosgrove and Black 2013; Twerenbold et al. 2003; Earhart et al. 2014; Del Coso et al. 2016; Hew-Butler et al. 2006) there is currently little evidence that replacing sodium during exercise will improve performance in the same way that consuming adequate carbohydrate or fluid will.
It is important to realize that the concentration of sodium in sweat is much lower than in plasma (table 9.5) and that with little or no fluid intake during exercise the plasma sodium concentration will inevitably rise. A moderate intake of fluid during exercise to replace up to 70% of fluid loss due to sweating will reduce the rise in the plasma sodium concentration or maintain it at resting levels. However, if more aggressive fluid replacement, particularly with plain water, is undertaken, then sodium replacement will be useful to balance that fluid intake and maintain a stable blood osmolality and plasma sodium concentration. According to McCubbin and Costa (2018), only when athletes exercise for more than 4 hours, have sweat rates over 1.8 L/h and, most importantly, are likely to drink to replace more than 70% of their sweat losses does the process of sweat sodium testing and targeted replacement appear necessary (infographic 9.1). Even then, only those athletes with above-average sodium concentrations in their sweat (i.e., greater than 40 mmol/L or 1.0 g/L) are likely to need to focus on sodium replacement during exercise (figure 9.14). Besides, research suggests that humans have some stores of sodium in the body that can be added to or released back into the circulation as needed. Because of the size of these stores, becoming deficient in sodium during acute exercise seems highly unlikely. The main issue to address is maintaining hydration by appropriate but not overzealous fluid intake. The need for sodium replacement during exercise appears to be linked to the extent of fluid replacement, and it is intended to balance the changes in body water so that the plasma sodium concentration (and therefore osmolality) is kept reasonably stable.
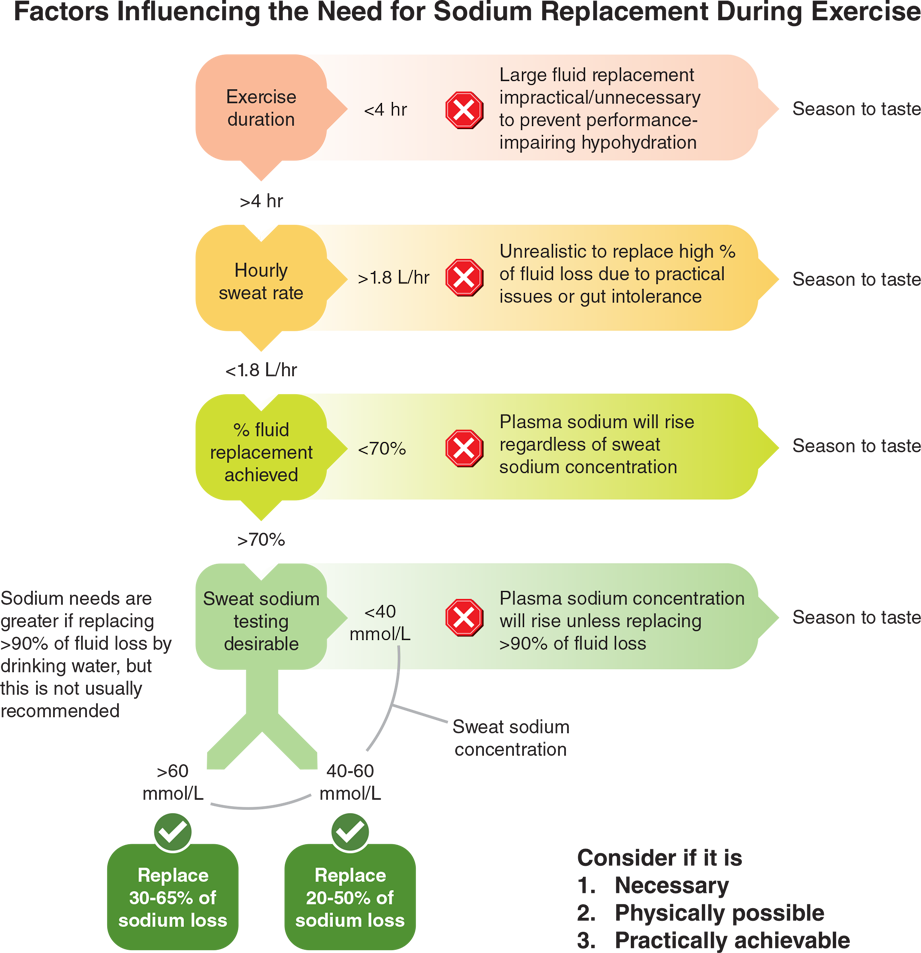
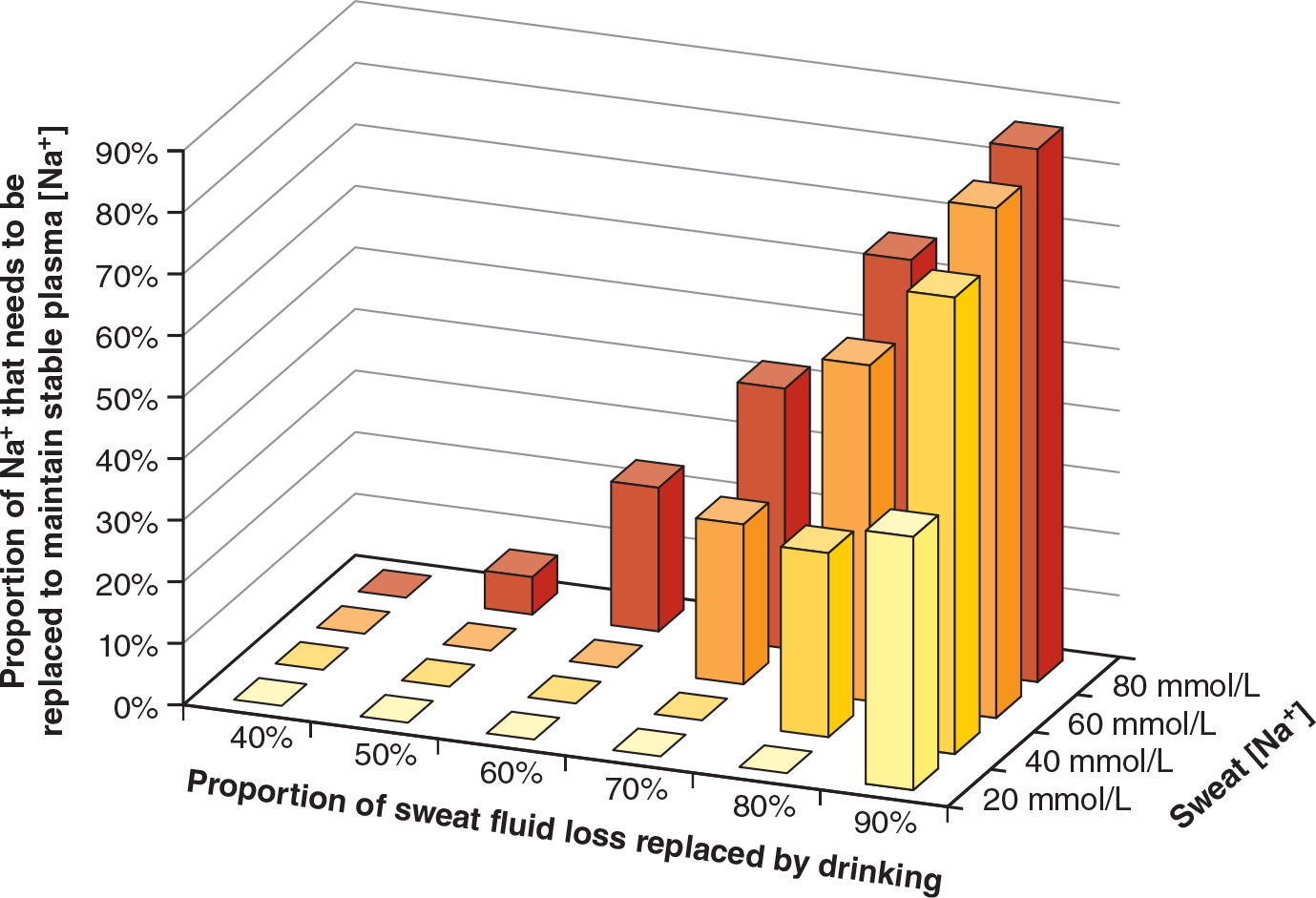
Data from McCubbin and Costa (2018).
You can understand why ideas about sodium replacement are changing when you consider the reasons for suggesting that sodium ingestion during exercise is not usually needed:
- Any athlete weighing 60 to 75 kg (132-165 lb) would have to lose 4 to 5 L of sweat before they would need to replace more than 70% of their fluid loss to prevent a loss of body weight of 2% or more that could result in a performance deficit.
- If the athlete’s sweat rate was 1.8 L/h, they would need to drink 1.3 L/h to achieve 70% replacement of their fluid loss. Even this is difficult to achieve in many sports due to potential gut discomfort and the limited opportunities for fluid intake during competition.
- The need for sodium replacement depends on the fluid replacement strategy; if athletes hydrate themselves appropriately (and not excessively) during exercise, they will not have a declining plasma sodium concentration.
- Sodium replacement is only needed to balance water turnover when fluid intake exceeds 70% of body weight loss, which will only occur when sweat rate is 1.8 L/h or more for at least 4 hours. Furthermore, this level of fluid replacement is only possible when gut tolerance and logistics allow it.
- Electrolyte (sodium) replacement is not critical for performance in most sports. It is only potentially beneficial in ultra-endurance events and only then to balance fluid replacement to prevent the development of hyponatremia.
The take-home message is that the only purpose for providing a targeted amount of sodium during exercise appears to be to maintain a stable plasma sodium concentration, and therefore osmolality, for any given volume of fluid intake. Given the composition of sweat, the plasma sodium concentration will only fall when athletes must replace most (greater than 70%) fluid losses to prevent dehydration and when whole-body sweat sodium concentration is above average (greater than 40 mmol/L or 1 g/L). Only in ultra-endurance exercise (i.e., events lasting more than 4 hours) is this likely to occur. In all other cases, athletes can simply season to taste (for improved palatability and to encourage drinking in reluctant drinkers) when it comes to sodium intake during exercise. The IOC consensus statement on recommendations and regulations for sport events in the heat (Racinais et al. 2023) is less conservative with regard to sodium replacement during exercise in the heat and simply suggests that for a salty sweater, it is possible to use sodium supplementation for exercise lasting longer than one hour. Given that the degree of fluid replacement is one of the main determinants of sodium replacement needs, athletes should first estimate their sweat fluid losses and replacement needs in relevant environmental conditions before deciding if sweat sodium testing and targeted replacement are necessary.
Does Sodium Ingestion During Exercise Cause Muscle Cramping?
The most common reason that athletes give for replacing sodium during exercise is to prevent or treat muscle cramping, with the view that the more sodium you lose, the more you need to replace. When muscle cramps do occur they can be painful and debilitating, which could obviously hamper performance or even force the athlete to withdraw from competition. Despite the many anecdotal stories of preventing cramps by ingesting salt tablets, scientific studies have failed to demonstrate this link (Miller et al. 2021). This evidence includes observational studies of people doing hard, repetitive, manual occupational work in hot conditions who commonly experienced cramping (Moss 1923; McCord and Ferenbaugh 1931; Talbott and Michelsen 1933; Talbott 1935; Dill et al. 1936), although this was more likely caused by excessive consumption of plain water than by dehydration or electrolyte losses. In some cases, taking salt tablets or drinking saline may have relieved cramping, but this is likely related to the balance of water and sodium rather than a frank sodium deficit. It is worth noting that muscle cramping often accompanies hyponatremia (defined as a serum or plasma sodium concentration below 135 mmol/L) in clinical settings (Adrogué and Madias 2000).
There are studies of athletes participating in prolonged endurance races where blood samples were taken and questionnaires completed by those who did or did not cramp. These studies found no relationship between hydration status, the use of salt replacement products, and plasma electrolyte concentrations between those who did and did not cramp—although in most cases the blood tests were not taken at the time of cramping but often several hours later (Maughan 1986; Schwellnus et al. 2004; Sulzer, Schwellnus, and Noakes 2005; Hofman and Stuempfe 2015). There have also been a few laboratory studies where sodium was given orally or intravenously with or without fatiguing exercise, and the level of electrical stimulation of the leg muscles needed to cause them to cramp was measured, but the researchers found that neither dehydration nor a large sodium deficit changed the risk of cramping (Lau, Kato, and Nosaka 2019, 2021).
The current consensus on exercise-associated muscle cramp is that it is most likely a complex syndrome, with multiple factors that can lead to changes in the function of the nerves that control muscle contraction (Maughan and Shirreffs 2019; Miller et al. 2021). These factors include local muscular fatigue and changes in the function of the nervous system itself related to pain, medications, or physical and psychological stress (infographic 9.2). Certainly, the modern view is that it is far too simplistic to blame cramping on one single factor such as an electrolyte deficit.
On the question of whether cramping might be related to an imbalance of (excess) water intake versus sodium loss, a few studies have reported that for people who were already dehydrated from exercise, consuming a large amount of plain water (as opposed to a sodium-containing drink) appeared to increase the risk of cramping when it was induced by electrical stimulation (Lau, Kato, and Nosaka 2019, 2021). While the reason for this remains unclear, it has been suggested that the drop in plasma sodium concentration and plasma osmolality that occurs when large volumes of plain water are consumed causes much of the water to rapidly enter the body tissues, resulting in nerve and muscle cell swelling. Clearly more research is needed on this issue before we can provide evidence-based practical recommendations. But even so, it seems that a “sodium deficit” is unlikely to be a potential cause of cramping in healthy people performing nonfatiguing exercise.
More Excerpts From Sport Nutrition 4th Edition With HKPropel AccessSHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- How do I integrate nutrition education into PE?
- How does the support of friends and family influence physical activity?
- What makes the Physical Best approach unique?
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?


