Communicate effectively with patients to enhance recovery
This is an excerpt from Psychology of Sport Injury by Britton W Brewer,Charles J Redmond.
Enhancing Patient - Practitioner Communication
As the preceding sections indicate, important outcomes are associated with the quality of patient - practitioner communication, which serves key informational and socioemotional functions in sport health care. However, significant discrepancies have been documented between the perceptions reported by patients and those reported by practitioners; therefore, we have much to gain by enhancing communication between the two parties. This goal has been pursued by means of two main approaches - interventions with practitioners and interventions with patients.
Interventions With Practitioners
Having recognized the advantages of physicians being attuned to the needs of their patients, medical schools have developed training programs to help doctors communicate more effectively with patients. These programs typically target common interpersonal courtesies (e.g., greeting patients by name, explaining procedures, saying goodbye), discussion of sensitive or difficult health topics, delivery of bad news, patient education, and how to help patients ask questions and remember key information. To help doctors develop such communication skills, training programs use video feedback and role-play exercises (Straub, 2012; S.E. Taylor, 2012). Similar coursework has been implemented with physical therapists and found effective in improving their communication skills (Ladyshewsky & Gotjamanos, 1997; Levin & Riley, 1984).
Although communication skills are recognized as vital to the practice of sport health care (Ray, Terrell, & Hough, 1999), relevant training for sport health care professionals has not reached the level of that found in medical schools on a consistent basis. With an eye toward addressing this gap, Gordon, Potter, and Ford (1998) proposed an extensive psychoeducational curriculum for sport health care professionals that prominently featured both lecture and applied experiences devoted to building communication skills in the context of sport health care. However, this curriculum has remained in prototype form and has not been implemented on a widespread basis. Even so, many sport health care professionals do receive some training in relevant communication skills through coursework in counseling. Basic counseling skills overlap heavily with the communication skills used in sport health care and therefore can help sport health care professionals build effective working alliances with patients.
In the context of sport health care, working alliances are relationships in which professionals and athletes collaborate to help athletes manage their injuries. A working alliance is designed to create an environment of trust and unified purpose, thus forging an emotional bond between the sport health care professional and the athlete and ensuring that the two parties are in agreement with respect to the goals and methods of treatment (Petitpas & Cornelius, 2004). Based on the influential work of Carl Rogers (1957), Petitpas and Cornelius suggested that an effective working alliance with an athlete depends on the practitioner's ability to communicate genuineness, acceptance, and empathy. Practitioners exhibit genuineness when they are true to themselves, aware of and open to appropriately sharing their feelings, and able to display nonverbal communication that is consistent with their verbal communication. Practitioners convey acceptance when they demonstrate unconditional positive regard for athletes and show respect for them regardless of what they do, think, or feel. Finally, practitioners display empathy when they show understanding of athletes' feelings and experiences from the athletes' perspectives. By communicating genuineness, acceptance, and empathy to athletes with injuries, sport health care professionals can facilitate the creation of an atmosphere of trust, caring, and understanding in which a working alliance can grow and thrive (Petitpas & Cornelius, 2004).
So, how exactly do sport health care professionals go about communicating genuineness, acceptance, and empathy? Learning and implementing basic counseling skills may help practitioners not only accomplish this goal but also help them put into practice their knowledge about patient - practitioner communication (e.g., informational and socioemotional functions, verbal and nonverbal modes). Basic counseling skills can be organized and described according to multiple models (e.g., Culley & Bond, 2007; Egan, 2014; Ivey, Ivey, & Zalaquett, 2013; Kottler, 2003; M.E. Young, 2012). These frameworks vary with respect to terminology and skill categorization but feature substantially similar behaviors. Specifically, in the context of sport health care, basic counseling skills can be divided into three groups based on their main function: attending to athletes and their concerns, exploring athletes' current concerns, and influencing athletes' thoughts or behaviors pertaining to their current concerns. These three types of skill are neither discrete nor mutually exclusive; rather, the boundaries between the categories are permeable - for example, there is no clear line at which exploring ends and influencing begins - and some skills (e.g., listening) overlap more than one category. Still, for the purpose of understanding, it is useful to examine each type individually.
Attending Skills
Also known as "invitational skills" (M.E. Young, 2012), attending skills involve verbal and nonverbal behaviors that convey the practitioner's interest in "tuning in" (Egan, 2014) or listening to what athletes with injury have to say. As the term implies, attending involves paying attention to athletes, which can be communicated nonverbally by maintaining direct eye contact (as appropriate, without staring), displaying receptive body language (e.g., encouraging gestures and facial expressions, relaxed posture, slight forward lean facing athletes at a socially appropriate conversational distance), and using appropriately varied vocal tones (Culley & Bond, 2007; Ivey et al., 2013; Kottler, 2003; M.E. Young). Verbal indicators, on the other hand, include inviting athletes to speak and staying on the topics that they bring up (Ivey et al.; M.E. Young). When practitioners give their attention to athletes and show their willingness to listen, they communicate genuineness and acceptance right from the start (Waumsley & Katz, 2013).
Exploring Skills
Through the process of exploration, sport health care professionals and athletes alike can learn more about the athletes' current concerns. Exploring typically begins when the practitioner asks questions. As discussed earlier in this chapter, the various types of question - closed, open, and focused - can generate different sorts of response from athletes. After the use of questioning gets the conversation started, the professional can help continue it by restating a few key words or phrases uttered by the athlete (e.g., "skiing career went kaput," "trained too hard") or by using brief statements that nudge athletes gently without intruding on their ideas (e.g., "tell me more," "uh huh," "and . . ."). Such encouragement not only stimulates conversation but also serves as an important form of active listening to the athlete's responses. Whereas passive listening involves merely hearing what another person says, active listening involves making a conscious effort to understand what the person is saying and communicating that effort back to the person, along with any understanding gained (Culley & Bond, 2007; Kottler, 2003).
Other forms of active listening include paraphrasing, reflecting feeling, and summarizing (Culley & Bond, 2007; Egan, 2014; Ivey et al., 2013; Kottler, 2003; M.E. Young, 2012). Paraphrasing involves repeating back to athletes key portions of their statements in an abbreviated form that uses at least some of their own words (e.g., "so the ‘swelling has gone down' but your knee is ‘even wobblier than it was before'"). Reflecting feeling involves identifying the athletes' emotions based on their verbal or nonverbal communication (e.g., "sounds like you're feeling pretty angry about how your surgery has turned out so far"). Whereas paraphrasing deals with thought content, reflecting feeling addresses emotional content; essentially, it involves paraphrasing athletes' expression of emotion. When sport health care professionals engage in summarizing, they offer athletes a pithy, organized account of the thoughts, feelings, behaviors, and meanings the athletes have conveyed in the interview.
The active listening skills of encouraging, paraphrasing, reflecting feeling, and summarizing serve multiple purposes in the process of exploration. Using these skills can be instrumental in helping sport health care professionals convey empathy to athletes and further demonstrate that the professionals are attending to the athletes (i.e., are interested in and willing to hear what they have to say). Practitioners can also use athletes' responses to these techniques to confirm or correct their understanding of what the athletes have been telling them.
Influencing Skills
For most sport health care professionals, the acquisition of attending skills and exploring skills provides a sufficient foundation for enhancing their ability to communicate with athletes. These skills enable practitioners to listen to patients, gain understanding of what they are experiencing, build rapport, express empathy, and solidify a working alliance. Although these skills are clearly nondirective, they are generally highly effective for collecting information and connecting with patients. Nevertheless, proficiency in the use of influencing skills can also be advantageous in the practice of sport health care. As implied by the term, influencing skills involve a more directive approach in which practitioners try to foster alternative ways for patients to think, feel, and act regarding their interactions in the world. There are three main clusters of influencing skills that vary in terms of whether they attempt to alter patients' cognitive processes, furnish patients with information, or prompt patients to act in some clearly defined way.
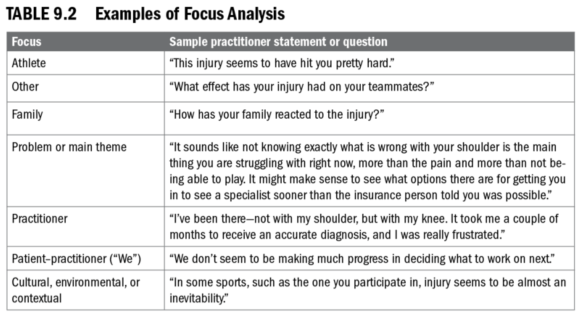
Two related influencing skills aimed at affecting patients' cognitive processes are reframing and focus analysis. Reframing, which is sometimes referred to as interpretation, involves encouraging athletes to think about a situation from a different, potentially more adaptive point of view (e.g., "So, you've told me a lot of ways that your injury has been problematic for you. What's on the other side of the ledger? What positive things have you experienced as a result of your injury?"). In a similar vein, focus analysis asks athletes to consider multiple aspects of a problem or situation. As shown in table 9.2, athletes can be asked to consider their injury using a patient (athlete) focus; an "other" focus; a family focus; a problem or main-theme focus; a practitioner focus; a patient - practitioner ("we") focus; or a cultural, environmental, or context focus. The locus (or type) of focus varies as deemed appropriate to facilitate understanding of the problems or situations experienced by the athlete. Although this type of analysis typically emphasizes helping athletes understand themselves and their concerns from their own perspective, it is sometimes valuable to broaden the focus in order to gain a fuller, more complete understanding of the pertinent issues and - when the "we" focus is involved - a better sense of what is happening in the patient - practitioner relationship (Ivey et al., 2013).
Another group of influencing skills involves providing patients with information designed to affect their thoughts or behaviors. Examples include providing advice or other information, self-disclosure, feedback, logical consequences, instruction or psychoeducation, and confrontation. Giving advice, a technique that is best used sparingly, involves recommending a course of action for the patient to take or furnishing the patient with new information that might be useful. Self-disclosure involves sharing current or past personal experiences with the patient (e.g., "Yeah, I know what you mean. I had to do rehab after ankle surgery a while back. It was pretty frustrating to see a lack of progress from day to day, but I guess I wanted it and stuck with it anyway."). Although self-disclosure can help build trust between patients and practitioners, the practitioner should be cognizant of whose needs are being served by disclosing the personal information.
Another skill in this group - feedback - involves letting patients know how their behavior is perceived by the practitioner and other people (e.g., "From what I've seen of your interactions with our staff, I have the impression that you've been quite angry these past few weeks"). A related skill - the use of logical consequences - involves informing patients about likely outcomes of their behavior (e.g., "As you might suspect, skipping your rehabilitation exercises may come back to bite you down the road in terms of a restricted range of motion and increased risk for injury in the future."). In using instruction, or psychoeducation, practitioners explicitly teach patients skills that may enhance their psychological state. Although instruction of some type accounts for a large part of what many sport health care professionals do, the skills they teach are often physical or technical in nature (as discussed later in this chapter). Psychoeducational content, of course, is most likely to be taught by sport health care professionals whose work with athletes is geared primarily toward effecting changes in psychological factors (e.g., cognition, emotion, behavior) - for example, sport psychology consultants and mental health specialists.
A third cluster of influencing skills includes techniques that issue a call to action - rather than providing information - intended to affect the patient's cognitions, emotions, behavior, or a combination thereof. Skills in this category include the use of confrontation, directives, goal setting, problem solving, stress management, reinforcement, and therapeutic lifestyle changes. In confrontation, which is far less adversarial than the term implies, practitioners note and bring to the patient's attention discrepancies in how the patient is thinking, feeling, and behaving. For example, if an athlete has repeatedly missed supervised rehabilitation sessions, the practitioner might say, "Throughout your rehabilitation, you've talked about how important it is for you to return to your sport as quickly as you can. Your actions, however, don't seem to match your stated goal. You're missing a lot of your appointments and seem to be going through the motions when you're here. What do you think is going on?" The next technique - using directives - is similar to giving advice or information in that it involves asking (rather than recommending or suggesting) that the patient take a particular course of action (e.g., "Today, I would like for you to do three sets of 15 reps at each station"). Because directives have the potential to undermine the patient's autonomy, they (like the sharing of advice, information, and self-disclosure) should be used with discretion.
The next three skills - goal setting (discussed in detail in chapter 8), problem solving, and stress management - are pragmatic influencing skills with which practitioners can help patients achieve clearly defined ends. In goal setting, for example, practitioners help patients set and pursue goals and evaluate their attainment of those goals. Similarly, in problem solving, practitioners guide patients through the process of defining problems, developing plans to address those problems, selecting the best plans, implementing the chosen plans, and evaluating the effectiveness of the chosen course of action (i.e., whether the plan worked). In stress management, practitioners help patients identify stressors and devise, implement, and evaluate plans to manage them.
The final two skills are reinforcement and therapeutic lifestyle changes. Reinforcement is a widely applicable skill that involves providing support and encouragement for patient behaviors deemed desirable (e.g., completing rehabilitation exercises, asking questions about rehabilitation). The practitioner can also help patients implement therapeutic lifestyle changes (e.g., regarding diet, smoking, exercise) to enhance both their general health and their injury-related health (Egan, 2014; Ivey et al., 2013; Kottler, 2003).
Learn more about Psychology of Sport Injury.
More Excerpts From Psychology of Sport InjurySHOP

Get the latest insights with regular newsletters, plus periodic product information and special insider offers.
JOIN NOW
Latest Posts
- How do I integrate nutrition education into PE?
- How does the support of friends and family influence physical activity?
- What makes the Physical Best approach unique?
- Strength training gimmicks . . . or not?
- How do vitamins and minerals support our bodies?
- Why do many people have difficulty losing weight?


